Abstract
Introduction: Acute painful episodes, frequently called sickle cell-related pain crises (SCPC), are a substantial cause of morbidity in sickle cell disease (SCD). Although hydroxyurea (HU) is known to decrease the frequency of SCPC in sickle cell anemia, many patients continue to experience acute painful episodes despite such therapy. P-selectin is an adhesion molecule expressed on activated vascular endothelial cells and platelets. It is a key molecule in the initiation of leukocyte rolling on the vessel wall that leads to firm attachment and extravasation to underlying tissues during inflammation. Upregulation of P-selectin on endothelial cells and platelets also contributes to the cell-cell interactions involved in the pathogenesis of SCPC. The SUSTAIN study evaluated the safety of SelG1, a first-in-class humanized anti-P-selectin antibody, and its effect on the frequency of SCPC in SCD patients.
Methods: We conducted a randomized, double-blind, placebo-controlled, multinational study. Patients were randomized to receive placebo, 2.5 mg/kg or 5.0 mg/kg SelG1; patients received their initial dose, a dose 14 days later, and then every 4 weeks through week 50 for a total of 14 doses. The primary efficacy endpoint was the annual rate of SCPC in the 5.0 mg/kg SelG1 group vs. placebo. A hierarchical testing procedure was employed (α = 0.05 for high dose vs. placebo, and if significant, low dose vs. placebo). An SCPC was defined as acute sickle cell-related pain that resulted in a visit to a medical facility and required a parenteral or oral narcotic or parenteral NSAID. Acute chest syndrome (ACS), priapism, hepatic and splenic sequestration were also included in this definition. A blinded, independent committee adjudicated all SCPC events. Key inclusion criteria included patients 16 to 65 years of age; diagnosis of SCD (HbSS, HbSC, HbSβ0 thalassemia or HbSβ+ thalassemia); and history of 2 to 10 SCPC in the previous 12 months. Patients receiving HU or erythropoietin were included if prescribed for the preceding 6 months and dose was stable for at least 3 months.
The randomization was stratified by historical SCPC in the prior year (2-4 or 5-10) and concomitant HU use (yes or no). Secondary endpoints included annual rate of days hospitalized, times to first and second SCPC and annual rate of uncomplicated SCPC (defined as typical SCPC other than ACS, priapism and hepatic or splenic sequestration) and ACS.
Results: 198 SCD patients were randomized for the 1-year study. The Intent-To-Treat (ITT) population included all randomized patients; 67, 66 and 65 patients in the 5.0 mg/kg, 2.5 mg/kg and placebo groups, respectively. Demographic parameters were evenly distributed in the treatment groups.
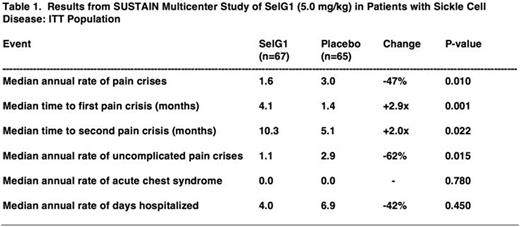
The primary endpoint, the annual rate of SCPC in the ITT population at 5.0 mg/kg vs. placebo, was reduced 47% (medians of 1.6 vs. 3.0, p = 0.010, Table 1). The SelG1 drug effect was dose-dependent as the annual rate of SCPC at 2.5 mg/kg vs. placebo was reduced 33% (medians of 2.0 vs. 3.0, p = 0.180). Time to first SCPC at 5.0 mg/kg vs. placebo was increased 2.9-fold (medians of 4.1 vs. 1.4 months, p = 0.001, Fig. 1) and time to second SCPC was increased 2.0-fold (medians of 10.3 vs. 5.1 months, p = 0.022, Fig. 2). The annual rate of uncomplicated SCPC at 5.0 mg/kg vs. placebo was reduced by 62% (medians of 1.1 vs. 2.9, p = 0.015). ACS events were rare in this study. The annual rate of days hospitalized at 5.0 mg/kg vs. placebo showed a non-significant, 42% reduction (medians of 4.0 vs. 6.9, p = 0.450).
Adverse events that occurred in 5% or more of patients in an active dose group and were elevated over placebo by at least 2-fold were arthralgia, pruritus, vomiting, chest pain, diarrhea, road traffic accident, fatigue, myalgia, musculoskeletal chest pain, abdominal pain, influenza and oropharyngeal pain. There were no apparent increases in infections with SelG1 treatment. Five deaths occurred during the study, 2 at 5.0 mg/kg, 1 at 2.5 mg/kg and 2 in placebo; no deaths were deemed related to study drug.
Conclusions: The P-selectin inhibitor SelG1 significantly reduced SCPC and appeared to be safe and well tolerated. Significant improvements were also achieved for several secondary endpoints including increases in times to first and second SCPC. Chronic inhibition of P-selectin with once a month IV dosing of SelG1 represents a novel and potentially new disease-modifying, prophylactic treatment option for patients with SCD. clinicaltrials.gov: NCT01895361
Kutlar:Novartis Pharmaceuticals: Research Funding. Kanter:Novartis: Consultancy. Rollins:Selexys Pharmaceuticals: Equity Ownership, Other: Previous Employment. Stocker:Selexys Pharmaceuticals: Equity Ownership, Other: Previous Employment. Rother:Selexys Pharmaceuticals: Equity Ownership, Other: Previous Employment.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal