In this issue of Blood, Linkins et al report on a prospective cohort study evaluating the combination of 4Ts (magnitude of thrombocytopenia, timing of onset of thrombocytopenia, thrombosis or other clinical sequelae, and the likelihood of other causes of thrombocytopenia) score and platelet factor 4/heparin particle gel immunoassay (PF4/H-PaGIA) for diagnosis and management of heparin-induced thrombocytopenia (HIT).1
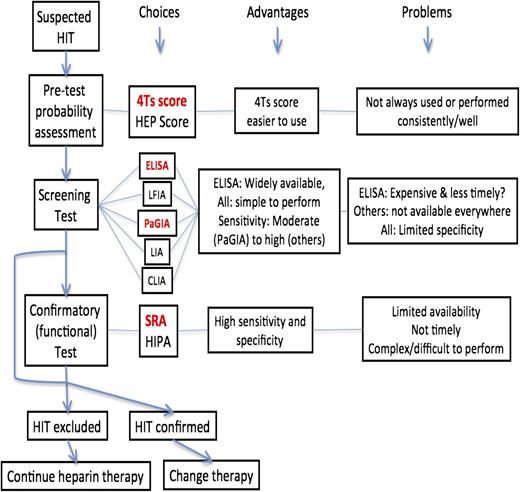
A simplified outline of HIT diagnosis or exclusion and consequent actions. The study by Linkins et al1 addresses some of the possible choices (refer to bold red font text). CLIA, chemiluminescence assay; HEP, HIT expert probability score; HIPA, heparin-induced platelet activation assay; IgG, immunoglobulin G; LIA, latex particle-enhanced immunoturbidimetric assay; LFIA, lateral flow immunoassay.
A simplified outline of HIT diagnosis or exclusion and consequent actions. The study by Linkins et al1 addresses some of the possible choices (refer to bold red font text). CLIA, chemiluminescence assay; HEP, HIT expert probability score; HIPA, heparin-induced platelet activation assay; IgG, immunoglobulin G; LIA, latex particle-enhanced immunoturbidimetric assay; LFIA, lateral flow immunoassay.
HIT leading to thrombosis is a greatly feared complication of heparin anticoagulant therapy. Missing a diagnosis of HIT has potentially lethal outcomes, and the consequences of overdiagnosing HIT are potentially as severe. Patients who do not have HIT are at risk for thromboembolic events if taken off heparin and at risk of major bleeding events while receiving nonheparin anticoagulants. Critically, rapid exclusion of HIT is needed to determine which patients can continue to safely receive heparin and rapid diagnosis of HIT to determine which patients must be moved to an alternate anticoagulant. HIT diagnosis relies on a combination of clinical suspicion and laboratory testing (recently reviewed by Cuker2 ); however, both have several limitations, and their combination thus offers the best solution for accurate diagnosis.
Clinical evaluation by means of a 4T score is the current gold standard approach, although other clinical evaluation tools also exist, such as the HIT expert probability score.2-4 The 4Ts score allocates points for 4 features (thrombocytopenia, timing of platelet count fall, thrombosis or other sequelae, and other causes for thrombocytopenia) for a maximum total possible score of 8. There are, however, several problems with this process. First, each of these features, even if present, may not actually be due to HIT; thus, the positive predictive value of even a high score is modest at best (64%; 95% confidence interval [CI], 40-82%). Second, the 4Ts score is inconsistently applied, so that different scores may be determined by different operators (ie, has limited interobserver reliability). Third, some features are not always apparent, and several gray zones exist (eg, there may be missing platelet count data points, and the history of recent heparin exposure may be unclear). On the other hand, in a meta-analysis of 13 studies, the negative predictive value of a low probability 4Ts score was high at 99.8% (95% CI, 97.0-100.0%) and remained high irrespective of several study variables.3
There are several options for laboratory testing for HIT.2 The gold standard is the serotonin release assay (SRA), a functional assay that detects antibodies that activate platelets in a heparin-dependent manner. The test procedure is technically difficult, uses radio-isotopes, has limited availability, and is quite time consuming. Although the test has high sensitivity and high specificity, it is typically not possible to obtain an immediate SRA assay, leading to development of a plethora of rapid assays with moderate to high sensitivity (0.9-1.0) and moderate specificity (0.7-0.95) for HIT.2 These assays comprise enzyme-linked immunosorbent assay (ELISA), lateral flow immunoassay, PaGIA, latex particle-enhanced immunoturbidimetric assay, and chemiluminescence assay.2 Their main advantages are they are rapid (results available within 10-30 minutes for all but ELISA), easy to perform, and can be performed immediately. Their limitations are moderate specificity, and they may not be available everywhere, depending on manufacturer distributions and regulatory clearances.
Linkins et al report on a prospective cohort study evaluating the combination of 4Ts score and 1 of these assays, PF4/H-PaGIA, plus ELISA testing, for HIT diagnosis and management. This study, representing 5 years of patient recruitment and analysis and a substantive number (538) of patients, reports several important findings. Sensitivity of the 4Ts score was 81.3% (95% CI, 67.7-94.8%) and specificity was 63.8% (95% CI, 59.5-68.0%). Expert and nonexpert 4Ts scores completed in duplicate showed only moderate agreement (κ = 0.43; 95% CI, 0.29-0.57). These findings confirm the limitations of the 4Ts score noted previously. The sensitivity of the PF4/H-PaGIA was 100% (95% CI, 89.1-100%) and specificity was 89.8% (95% CI, 87.1-92.5%). In regard to performance of the combination of 4Ts score and PF4/H-PaGIA, a negative PF4/H-PaGIA result reduced the pretest probability of HIT as determined by the 4Ts score from 1.9% to 0% (95% CI, 0-1.3%) in the low group, from 6.7% to 0% (95% CI, 0-2.7%) in the intermediate group, and from 36.6% to 0% (95% CI, 0-14.3%) in the high group, meaning a negative PF4/H-PaGIA was reasonably inconsistent with HIT. Alternatively, a positive PF4/H-PaGIA result increased the probability of HIT to 15.4% (95% CI, 5.9-30.5%), 42.3% (95% CI, 23.4-63.1%) and 88.2% (95% CI, 63.6-98.5%) in each of these groups, respectively.
Although others have prospectively evaluated the combination of 4Ts score with a rapid immunoassay to diagnose HIT, the current study is the first to use this combination to guide clinical management of patients with suspected HIT in real time. The main take-home messages from this impressive study are that a negative PaGIA in a patient with low/intermediate 4Ts score excludes HIT with a high level of confidence and that a low 4Ts score alone is insufficient to exclude HIT.
However, this study provides data with just 1 rapid assay. This assay is not available everywhere. In addition, during the study, a worldwide shortage ensued, complicating the study. In real-world use, the consequences could be more drastic. Finally, the reproducibility of different batches of PaGIA has been questioned.5 Accordingly, readers of Blood are referred elsewhere for studies assessing additional rapid assays for utility in HIT,2 as well as comparative studies evaluating several rapid HIT assays in parallel (eg, Vianello et al).6 This study limitation is summarized in the figure.
In conclusion, there are failures in both pretest probability assessment (eg, the 4Ts score) and laboratory rapid assays, but concurrent failures in both are likely to be rare; hence, the combination of both (low or intermediate 4Ts plus negative rapid assay) would expectedly make effective negative exclusion panels. Of course, making clinicians undertake 4Ts pretesting and doing this consistently and well represents another difficulty. Also, there remains ongoing problems of what to do with low 4Ts scores with positive rapid assays and the dangers of overcalling HIT, which to a large extent will still likely remain, despite the study findings and the authors’ expert guidance (refer to study algorithm). Finally, additional caution is indicated due to laboratory difficulties in terms of test performance as evidenced by interlaboratory test variation (eg, Smock et al).7
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal