Abstract

Introduction: Hematopoietic stem cell transplantation (HSCT) is being increasingly used as curative therapy for severe disorders of the hematopoietic system and transfusional iron overload (TIO) contributes considerably to treatment-related morbidity and mortality after HSCT. Management of iron overload in the post-HSCT setting may be complicated since the use of therapeutic phlebotomies is often not feasible due to ongoing anemia and compliance to deferoxamine is low. Studies that evaluate the safety dose of deferasirox (DFX), which is the most commonly used chelation therapy, in this setting are limited.
Purpose & Methods: This is a prospective, phase 2, multicenter, single-arm study to evaluate the efficacy and safety of iron chelation with oral DFX in beta-thalassemia major (TM) patients who have undergone HSCT. The study was conducted in 7 centers from Turkey. The primary objective was to evaluate if DFX could provide clinically safe chelation in a target pool of 26 pediatric patients with TIO within a minimum of 6 months and maximum of 2 years after related/unrelated HSCT. Patients had to be transfusion-independent and have iron overload at screening defined by serum ferritin (SF) of >1000 μg/L or cardiac MRI T2* <20 ms or liver iron concentration (LIC, by MRI R2) of ≥5 mg/g. The study included male and female TM patients ≥2 to <18 years old who had undergone HSCT with a washout period from immunosuppressive therapy of at least 3 months. Patients received DFX at an initial dose of 10 mg/kg/day with up titration every 3 months by 5 mg/kg/day per investigator judgment to a maximum of 20 mg/kg/day. Therapy continued for 52 weeks or until SF reached below 500 μg/L. Aside from AE monitoring, assessments were undertaken at baseline and every 28 days (unless closer assessments were need for dose initiation and adjustment) and included complete blood counts, biochemistry and urinalysis, and SF. MRI assessment of liver (R2) and cardiac (T2*) iron were also conducted at baseline and 52 weeks.
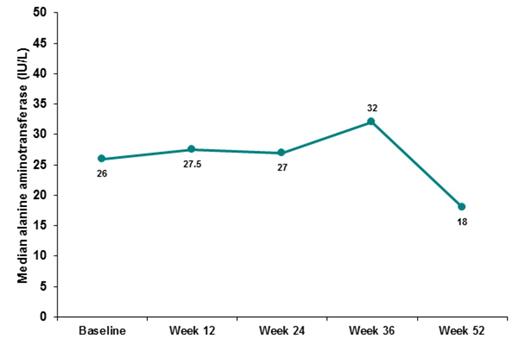
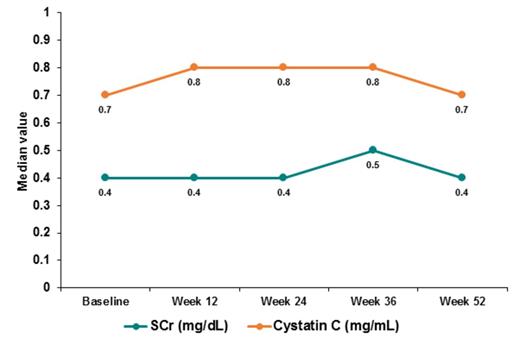
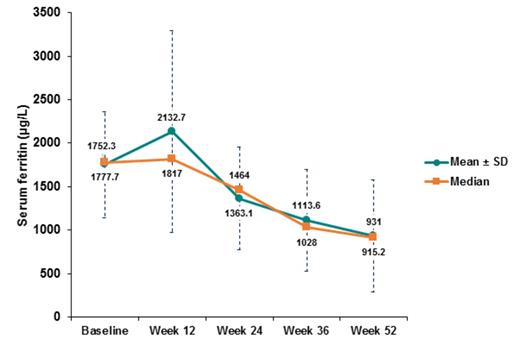
Results: Interim data from the first 18 of 26 patients (mean age 8.3 years, 66.7% males) who completed 12 months follow up are presented in this analysis. A total of 97 AEs were recorded in the 18 patients. The majority of AEs were of Grade I (n=57) or II (n=34) severity. Five (5.2%) were suspected to be related to study drug and 6 AEs (6.2%) were considered serious. Five (5.2%) AEs resulted in study drug temporary interruption or dose adjustment, 2 (2.1%) required hospitalization, 54 (55.7%) required concomitant medication, while 36 (37.1%) had no action taken. Three patients had dose decrease due to AEs. The dose was re-escalated up to 20 mg/kg/day after the AEs resolved. In total, 11 (61.1%) patients achieved 20 mg/kg/day. Only one patient dropped out due to progressive ALT increase. Median ALT level decreased from 26 IU/L (range: 10-117) at baseline to 18 IU/L (range: 9-101) at week 52. The median SCr was similar at baseline 0.4 mg/dL (range: 0.2-0.6) and week 52 0.4 mg/dL (range: 0.2-0.8). Median cystatin C was similar at baseline 0.7 mg/mL (range: 0.6-0.9) and week 52 0.7 mg/mL (range: 0.5-1.1) (Figure 1A-B). Five patients had proteinuria at baseline and increased proteinuria compared to previous visit by dipstick analysis was described in 7 (38.9%) patients, irrespective of DFX dose by 52 weeks. No patient with proteinuria required any dose adjustments by 52 weeks. SF significantly and consistently decreased throughout the 52 weeks from a median of 1752.3 μg/L (range: 873.7-2716) to 915.2 μg/L (range: 250.1-2740), p<0.001 (Figure 2). At week 52, 6 (33.3%) patients had reached SF <500 μg/L. LIC also significantly decreased from a median of 9.9 mg/g (range: 4.8-43) to 4.1 mg/g (range 0.9-8.5), p<0.001. Cardiac T2* increased from a median of 26.1 ms (range: 18.7-41) to 28.8 ms (18.5-44), p=0.605.
Conclusions: Our preliminary results showed that DFX up to 20 mg/kg/day is safe and effective in reducing iron burden for TM patients following HSCT. This was evident through significant reductions of systemic, hepatic and cardiac iron overload. Final data from the completed study should confirm these findings and establish the role for DFX in this patient population.
Dag:Novartis: Employment. Birkent:Novartis: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal