Abstract

Introduction: Hereditary hemolytic anemias (HAs) is a group of heterogeneous disorders mainly due to defects of red cell (RBC) membrane and metabolism. HAs of RBC membrane are classified according to the morphological appearance on a blood smear: the more common are hereditary spherocytosis (HS), elliptocytosis, followed by stomatocytosis (dehydrated, DHSt and overhydrated, OHSt). Among RBC enzyme defects associated with chronic hemolysis, pyruvate kinase (PK) deficiency is the most common, followed by glucose-6-phosphate isomerase (GPI), pyrimidin 5' nucleotidase (P5'N), and more rarely, other enzymes deficiencies. Because of the rarity and heterogeneity of these diseases, diagnosis may be often challenging despite the availability of a battery of laboratory tests. Ektacytometry, and more recently, laser-assisted optical rotational cell analyser (LoRRca MaxSis, Mechatronics Instruments, NL), able to measure RBC deformability in osmotic gradient conditions (Osmoscan), is reported to be a useful tool in the detection of RBC membrane disorders and in particular for the differential diagnosis of HSt. Few data are available in other haemolytic anemias.
Methods: We evaluated the diagnostic power of laser-assisted optical rotational cell analyser in 84 cases with RBC membrane disorders (69 HS, 7 HE, 7 DHSt, 1 OHSt) and 26 enzymopathies: 19 PK deficiency (14 not splenectomised), 4 GPI deficiency and 3 P5N deficiency. Moreover, we analysed 8 congenital diserythropoietic anemia type II (CDA II), of whom 3 not splenectomised. A reference curve interval was obtained from 89 healthy controls. The evaluated parameters were: Omin (osmotic value at which the EI reaches its minimum, coinciding with the 50% hemolysis in osmotic fragility assays), EImax (maximal deformability obtained near the isotonic osmolality), and Ohyper (osmotic value at which the EI reaches half of its maximum value, representing cellular hydration status).
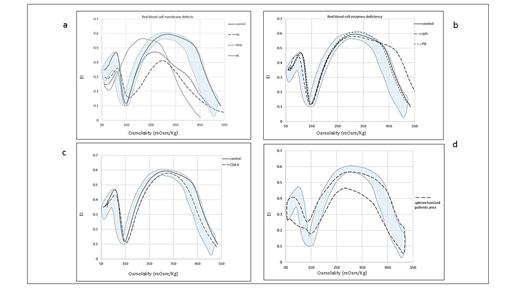
Results: Considering membrane defects, all the 69 HS, regardless the biochemical defect, showed typical altered ektacytometry curves, with a decreased EImax (0.516±0.05 vs 0.595±0.008 for controls, p<0.0001) and right shifted Omin (167±11.4 vs 143.7±7.2, p<0.0001); the 7 HE cases displayed a trapezoidal feature and a decreased EImax (0.547±0.05 vs 0.595±0.008, p<0.001). Among the hereditary stomatocytosis, the 7 DHSt were characterized by a left-shifted curve (Fig 1a).
Concerning RBC enzymopathies, we found that all the GPI deficient cases showed altered enlarged Osmoscan curves associated with significant increased Ohyper (539±36 vs 462±13.4, p<0.0001), whereas not splenectomised patients with PK deficiency showed an Osmoscan curve characterised by an increased EImax (0.601±0.01 vs 0.595±0.008), although not significant (Fig 1b). Osmoscan curve in not splenectomised CDAII falls in the low reference area of normal controls. However, Omin and EImax were signifificantly different from HS patients thus permitting a differential diagnosis (Omin 149.3 ±3.0 vs 167±11.4, p<0.01; EImax 0.578±0.02 vs 0.516±0.05, p<0.05) (Fig 1c).
We separately analysed splenectomised and not splenectomised patients. Interestingly, for some diseases (PK, P5N, CDAII and OHSt) Osmoscan curve after splenectomy, falls in a defined atypical area, regardless the pathology (Fig 1d).
Conclusion: The Osmoscan curves were diagnostic for all the HS and HE cases analysed, with Omin and EImax parameters significantly different from controls. DHSt cases always showed typical left-shifted curve. Interestingly, Ohyper was firstly described increased in GPI deficiency, offering a new diagnostic tool for this rare enzyme defect. The interpretation of Osmoscan requires caution in splenectomised cases as splenectomy may interfere with the RBC deformability. In conclusion, the Osmoscan analysis performed by LoRRca Maxsis represents a useful and feasible first step screening test in the diagnosis of RBC membrane disorders and other rare haemolytic anemias.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal