Abstract
Introduction
The standard primary endpoint in clinical trials of chronic lymphocytic leukemia (CLL) is progression-free survival (PFS). Given the increasingly long follow up required to detect differences in PFS between treatment arms in the era of more efficient therapeutics, valid surrogate endpoints are urgently needed to reduce clinical trial duration, thereby accelerating drug development, reducing costs and allowing patients (pts) earlier access to novel treatment options.
Pts with CLL who achieve levels of minimal residual disease (MRD) of <1 clonal cell/10.000 leukocytes in peripheral blood (PB) as determined by multicolor flow cytometry or allele-specific oligonucleotide real-time quantitative polymerase chain reaction (ASO-RQ-PCR) at the end of initial treatment are considered MRD negative, and have been shown to experience significantly improved PFS.
This analysis aimed to support the evaluation of MRD response at the end of treatment as a surrogate endpoint for PFS in CLL, based on a retrospective analysis of 3 multicenter, randomized, Phase 3 clinical trials.
Methods
MRD was prospectively assessed in PB of treatment-naive pts with CLL that participated in the German CLL Study Group CLL8, CLL10 and CLL11 multicenter, randomized, open-label, Phase 3 clinical trials, which included induction treatment followed by observation. The primary endpoint of each study was investigator-assessed PFS. MRD was quantified by 4-color flow cytometry in CLL8 and CLL10, and ASO RQ-PCR in CLL11. Both methods had a detection threshold of 1 CLL cell/10,000 leukocytes. Pts who had no MRD result but had disease progression or died shortly after 6 treatment cycles (within 90 [CLL8 and CLL10] or 56 [CLL11] days of last dose) were included and classed as MRD positive. A meta-regression model was developed to predict treatment effect on PFS using treatment effect on MRD. Log ratio was selected as the most reliable representation of MRD response based on the best model fit. To ensure no systemic bias with pt selection, demographic characteristics and efficacy results for the pt population used in the MRD analysis were compared with the respective intent-to-treat populations for each study.
Results
PB MRD levels at the end of treatment (CLL8 and CLL10, 75-195 days after last dose; CLL11, 56-190 days after last dose) were assessed in 393, 336, and 474 pts from CLL8, CLL10 and CLL11, respectively. PFS events occurred in 24% to 51% of pts assessed for MRD assigned to the experimental arm and in 34% to 67% assigned to active control treatment. Key efficacy data for the 3 trials are shown in Table 1.
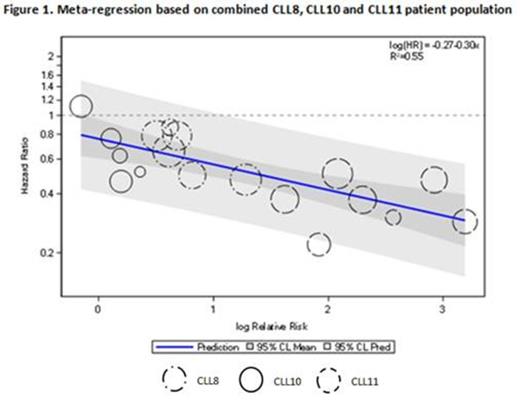
To fit a meta-regression model, each study was split into subgroups according to region (CLL8), country (CLL11) or randomly (CLL10). For each subgroup, the PFS hazard ratio (HR) was plotted against the ratio of MRD response rates (MRD negative rate in experimental arm to MRD negative rate in control arm, on a log-scale), and a regression line fitted to reflect the relationship between the two parameters (Figure 1). Circle size represents the weighting of each subgroup to the overall model; least variability in PFS HR have the largest circles. Clustering of circles by study reflects the overall treatment effect (for both MRD and PFS) in the studies. A statistically significant relationship between improved MRD response rates and reduction in the risk of disease progression or death was observed (for each unit increase in log of the ratio of MRD response rates, the log of PFS HR decreases by -0.299; 95% CI, -0.441 to -0.157; p=0.0004).
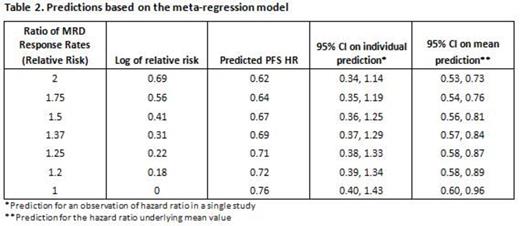
Predictions based on this meta-regression model suggest that risk of progression or death decreases as the ratio of MRD response rates (MRD relative risk: MRD-negative rate in experimental arm/MRD-negative rate in control arm) increases (Table 2); i.e. a larger difference in MRD-response rates leads to lower PFS HR.
Conclusion
A surrogate endpoint (MRD) should not only provide prognostic value for the specific clinical outcome (PFS), but also evidence that treatment effect on the surrogate endpoint (MRD) reliably predicts treatment effect on the clinical outcome (PFS). Results of the meta-regression model show a significant association between treatment effect on MRD and treatment effect on PFS with regard to chemoimmunotherapy. The findings also suggest that treatment effect on PFS can be predicted based on treatment effect on MRD response. This model supports the use of MRD as a surrogate for PFS in pts with CLL.
Dimier:Roche: Employment. Delmar:F. Hoffmann-La Roche, Ltd.: Employment, Equity Ownership. Ward:F. Hoffmann-La Roche Ltd: Employment. Morariu-Zamfir:F. Hoffmann-La Roche Ltd: Employment. Fingerle-Rowson:Roche: Employment, Equity Ownership. Fischer:Roche: Other: Travel Grants. Eichhorst:Mundipharma: Consultancy, Research Funding, Speakers Bureau; AbbVie: Consultancy; Roche: Consultancy, Research Funding, Speakers Bureau. Goede:Mundipharma: Honoraria; Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel support, Research Funding; GSK: Honoraria; Bristol-Myers Squibb: Honoraria. van Dongen:InVivoScribe: Patents & Royalties: Licensing of IP and Patent on BIOMED-2-based methods for PCR-based Clonality Diagnostics. Royalty income for EuroClonality-BIOMED-2 Consortium.; DAKO: Patents & Royalties: Licensing of IP and Patent on Split-Signal FISH. Royalties for Dept. of Immunology, Erasmus MC, Rotterdam, NL; Cytognos: Patents & Royalties: Licensing of Patent on detection of IgE+ B-cells in allergic diseases. Royalties for Dept. of Immunology, Erasmus MC, Rotterdam, NL; Cytognos: Patents & Royalties: Licensing of IP on Infinicyt software, Patents on EuroFlow-based flowcytometric Diagnosis and Classification of hematological malignancies, Patents on MRD diagnostics, and Patents on PID diagnostics. Royalty income for EuroFlow Consortium.; BD Biosciences: Other: Educational Lectures and Educational Workshops (+ related travelling costs). Laboratory Services in the field of technical validation of EuroFlow-OneFlow antibody tubes in dried format. Provided by the Laboratory of Medical Immunology, Erasums MC, Patents & Royalties; Roche: Consultancy, Other: Laboratory Services in the field of MRD diagnostics, provided by the Laboratory of Medical Immunology, Dept. of Immunology, Erasmus MC, Rotterdam, NL; Immunostep: Patents & Royalties: Licensing of IP and Patents on immunobead-based dection of fusion proteins in acute leukemias and other tumors. Royalties for Dept. of Immunology, Erasmus MC and for EuroFlow Consortium. Ritgen:Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding. Böttcher:Celgene: Research Funding; AbbVie: Consultancy, Honoraria, Other: Travel, accommodation, expenses, Research Funding; Roche: Consultancy, Honoraria, Research Funding; Beckton Dickinson: Honoraria. Langerak:InVivoScribe: Patents & Royalties: Licensing of IP and Patent on BIOMED-2-based methods for PCR-based Clonality Diagnostics. ; DAKO: Patents & Royalties: Licensing of IP and Patent on Split-Signal FISH. Royalties for Dept. of Immunology, Erasmus MC, Rotterdam, NL; Roche: Other: Lab services in the field of MRD diagnostics provided by Dept of Immunology, Erasmus MC (Rotterdam). Hallek:Janssen: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding; Gilead: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding; Roche: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding; Celgene: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding; Pharmacyclics: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding; Mundipharma: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding; Boehringher Ingelheim: Honoraria, Other: Speakers Bureau and/or Advisory Board; AbbVie: Honoraria, Other: Speakers Bureau and/or Advisory Board, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal