Abstract
Introduction
EBV reactivation and associated diseases have been well recognized as one of the life threatening complications after SCT, which leads to the establishment of prophylactic and preemptive treatment for EBV viremia. However since then, few epidemic data was shown in SCT recipients, especially in China.
Patients and Methods
An observational data base study was conducted in patients with hematological disorders who received allo-SCT from Jun 2011 through Jun 2014. EBV-negative status was confirmed before transplant for both donors and recipients. EBV-DNA was screened weekly until Day 100 post SCT by qPCR, and then every 2-4 weeks until 1 year. Additional tests were carried out when clinically indicated. All patients received ganciclovir during conditioning regimen, and then switched to acyclovir or valaciclovir after stem cell infusion until 1 year post SCT. Ganciclovir and/or foscarnet were used when DNAemia developed, as well as rituximab for high risk patients such as high viral load or persistent DNAemia.
Results
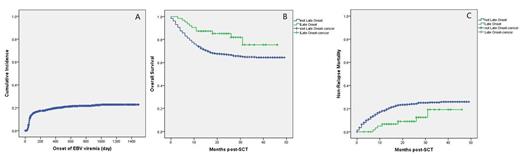
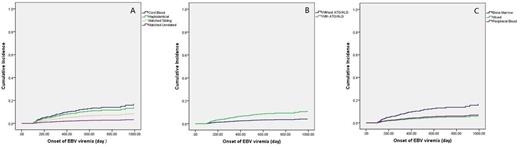
This study recruited 892 evaluable cases, including 91 cases of benign diseases and 801 cases of malignancies. Until Jun 2015, EBV-DNA was detected in 178 cases with a median duration of 55 days (16-990days) post SCT, and the long-term cumulative incidence of DNAemia was 22.8¡À1.6%(Fig 1A). Log-rank test showed the onset of EBV-DNAemia had impact on neither OS nor NRM. However, For patients with late-onset EBV viremia (later than 100 days post-SCT), superiority of 3 year-OS (75.6¡À7.9% vs 65.2¡À1.8%, P=0.013) and 3 year-NRM (19.2¡À8.0% vs 25.4¡À1.7%, P=0.028) were observed(Fig 1B and Fig 1C). Furthermore, late-onset of EBV viremia was confirmed as independent protective factor for both OS£¨RR 0.466 [95%CI 0.253-0.859], P=0.014) and NRM (RR 2.271 [95%CI 1.056-4.882], P=0.036) in multivariate analysis. Cox model analysis revealed that the haploidentical donor£¨RR 4.745 [95%CI 1.624-13.866], P=0.004) and the use of ATG/ALG were independent risk factors for late-onset of EBV viremia, as well as the graft of bone marrow (RR 2.188 [95%CI 0.991-4.835], P=0.053) with a marginal significance(Figure 2).
Conclusion
This work showed the cumulative incidence of EBV viremia after allogeneic SCT was around 22.8% based on virus prophylaxis. As shown in multivariate analysis, late-onset of EBV viremia had independent impact on OS and NRM. Haploidentical donors, the use of ATG/ALG and graft type were independent risk factors for late-onset EBV viremia..
This work was funded by grants of Jiangsu Provincial Special Program of Medical Science (BL2012005), Jiangsu Province¡¯s Key Medical Center (ZX201102) and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
A. Cumulative incidence of EBV DNAemia; B. Comparison of OS between early-onset and late-onset of EBV viremia; C. Comparison of NRM between early-onset and late-onset of EBV viremia;
A. Cumulative incidence of EBV DNAemia; B. Comparison of OS between early-onset and late-onset of EBV viremia; C. Comparison of NRM between early-onset and late-onset of EBV viremia;
Independent risk factors for late-onset of EBV viremia: A. the impact of donor types; B. the impact of conditioning regimens with and without ATG/ALG; C. the impact of graft types.
Independent risk factors for late-onset of EBV viremia: A. the impact of donor types; B. the impact of conditioning regimens with and without ATG/ALG; C. the impact of graft types.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal