Abstract
Objection:
Chronic lymphocytic leukemia (CLL) is a chronic lymphoproliferative disease characterized by highly clinical and biological heterogeneity. A number of biomarkers have been identified in predicting the overall survival (OS) over the last decades besides the traditional clinical staging. Recently, an international prognostic index (IPI) combing clinical staging and biomarkers was developed by the investigators of the Cochrane Haematological Malignancies Group. Due to genetic differences between Caucasic and Chinese CLL patients, our study was to validate the guiding function of IPI on Chinese CLL cases.
Method:
We performed a validation of the IPI proposed by the Cochrane Haematological Malignancies Group to stratify Chinese CLL patients prognostically in 225 CLL cases registered at our center. The five parameters (age, TP53 abnormalities, IGHV mutation status, b2-microglobulin and Binet stage) involved in the IPI were collected by clinical data, serum test, PCR and fluorescence in situ hybridization (FISH). Chi-square test, survival analysis, log-rank test and cox hazard regression analysis were utilized in the validation.
Result:
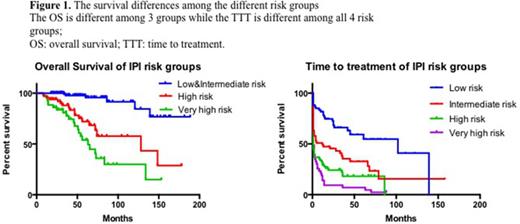
In the 225 Chinese CLL cases analysed in the validation, all five parameters involved in the IPI were associated with overall survival (OS) independently. The multivariate analysis demonstrated that age above 65 years old (HR 2.22; [1.15-4.30]; P=0.018), b2-microglobulin over 3.5 mg/L (HR 2.46; [1.22-4.94]; P=0.001), Binet staging B/C (HR 3.40; [1.02-11.33]; P=0.046), TP53 abnormalities (HR 2.72; [1.50-4.94]; P=0.012) and IGHV unmutation (HR 5.19; [2.51-10.77]; P<0.001) were OS related risk factors respectively. Then a total point score was calculated for each patient according to the grading system proposed by the Cochrane Haematological Malignancies Group investigators. There were 60 (26.7%) patients at low-risk (scoring 0-1), 57 (25.3%) patients at intermediate-risk (scoring 2-3), 65(28.9%) patients at high-risk (scoring 4-6) and 43 (19.1%) patients at very high-risk (scoring 7-10). The IPI allowed different prediction of time to treatment (TTT) in all groups (Fig. 1). The estimated median TTT were: 102 months for low-risk, 12 months for intermediate-risk and 1 month for high-risk group. However, the low-risk and intermediate-risk groups showed similar overall survival (P=0.424). Beyond that, significant difference was found between the intermediate, high and very high-risk groups. We combined the low-risk and the intermediate-risk groups into one to accommodate to the Chinese CLL cases. 117 (52%) patients were at low & intermediate-risk (scoring 0-3), thus leading to the significantly different prognostic value between groups (Fig. 1) . The estimated median survival times were: not reached for low&intermediate-risk, 63 months for high-risk and 128 months for very high-risk group.
Conclusion:
Our results basically validated the IPI proposed by the Cochrane Haematological Malignancies Group to prognostically stratify CLL patients in China, which confirmed the value of the novel prognostic index externally. However, a slight adaption was made to accommodate the Chinese cases better via the combination of the low-risk and intermediate-risk groups. We considered that a universally recognized prognostic model would be utilized to predict the disease progression and guide the treatment when initially diagnosed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal