Abstract
Introduction: BCR-ABL kinase mutations are the most common reason of resistance to tyrosine kinase inhibitors (TKIs) in chronic myeloid leukemia (CML) patients1. Hence, determination of BCR-ABL mutation status at the time of resistance, disease progression and subsequent drug switching is an integral component of North American and European clinical guidelines 1,2. Compound BCR-ABL mutations have been emerged as one of the major issues in TKI-based therapy of CML, which cause new patterns of drug resistance, including resistance to ponatinib 3. This study wascarried out to find out association of BCR-ABL mutations with treatment outcome in CML patients.
Materials & Methods: 150 CML patients were investigated for BCR-ABL mutations using direct sequencing as previously reported 4. SPSS version 19 (IBM, Chicago, IL, USA.) was employed for statistical analysis.
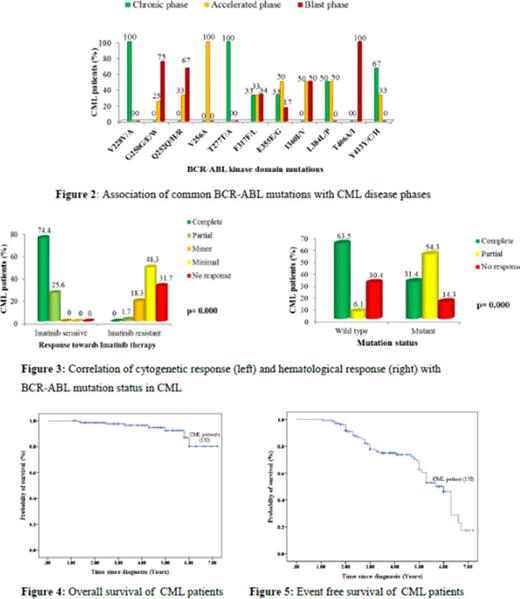
Results: 78 (52%) patients were males and 72 (48%) females, with median age 34 years (range: 9-62) (Table 1). Ninety (60%) were IM sensitive and 60 (40%) IM resistant. 72 mutations were detected in 28 (46.7%) patients, with 71.4% patients having compound (2-5) mutations. 14 mutations were detected in 7 IM sensitive patients in late chronic or advanced phases. E355G was the most common mutation (Fig 1). P-loop mutations were found only in IM resistant patients at advanced phases (Fig 2). Elevated TLC, advanced phases and suboptimal responses were associated with IM resistance and mutations. Higher complete hematological and complete cytogenetic responses were seen in patients without mutations (Fig 3). 7-year OS and EFS were 80.4% and 55.6%, respectively (Figs 4-5). Higher survivals were associated with IM sensitivity, low or intermediate Sokal risk, chronic phase, complete hematologic response and complete cytogenetic response.
Discussion: Our results show association of BCR-ABL mutations with IM resistance, disease progression and late chronic phase 1,4. Therefore, we recommend BCR-ABL mutation detection for late chronic phase CML patients as well. High frequency of compound mutations in IM resistant patients poses a threat to CML patients by complicated drug resistant patterns, including resistance to 3rd generation TKIs 3,6,7. Therefore, we recommend regular monitoring of CML patients for BCR-ABL mutations and associated drug response in all patients at risk of BCR-ABL mutations and drug resistance.
References:
1- Hochhaus A, Ernst T, Eigendorff E, La Rosée P. Causes of resistance and treatment choices of second- and third-line treatment in chronic myelogenous leukemia patients. Ann Hematol. 2015 Apr;94 Suppl 2:S133-40.
2- Baccarani M, Castagnetti F, Gugliotta G, Rosti G. A review of the European LeukemiaNet recommendations for the management of CML. Ann Hematol. 2015 Apr;94 Suppl 2:S141-7. 3- Zabriskie MS, Eide CA, Tantravahi SK, Vellore NA, Estrada J, Nicolini FE,et al. BCR-ABL1 compound mutations combining key kinase domain positions confer clinical resistance to ponatinib in Ph chromosome-positive leukemia. Cancer Cell. 2014 Sep 8;26(3):428-42.
4- Iqbal Z, Akhtar A, Akram AM, Khalid M, Shah IH, Aleem A, et al. Detection of Compound BCR-ABL Mutations in TKI Resistant CML Patients Including a Novel K245N Mutation Associated with Primary Nilotinib Resistance By Employing a Newly Developed Cost Effective BCR-ABL Sequencing Protocol. Blood Dec 2014; 124(21):1810.
5- Castagnetti F, Gugliotta G, Breccia M, Stagno F, Iurlo A, Albano F, et al. Long-term outcome of chronic myeloid leukemia patients treated frontline with imatinib. Leukemia. 2015 Jun 19. doi:10.1038/leu.2015.152. [Epub ahead of print]6- BCR-ABL1 compound mutations drive ponatinib resistance. Cancer Discov. 2014 Nov;4(11):OF13. doi: 10.1158/2159-8290.CD-RW2014-186.
7- Gibbons DL, Pricl S, Posocco P, Laurini E, Fermeglia M, Sun H, Talpaz M,Donato N, Quintás-Cardama A. Molecular dynamics reveal BCR-ABL1 polymutants as a unique mechanism of resistance to PAN-BCR-ABL1 kinase inhibitor therapy. Proc Natl Acad Sci U S A. 2014 Mar 4;111(9):3550-5.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal