Abstract
Background
Chronic myeloid leukemia (CML) is a myeloproliferative disorder which can present in one of the three disease phases; chronic phase, accelerated phase or blast crisis. Central nervous system (CNS) as a site of extramedullary blast crisis in CML is rare and when affected, it usually occurs concurrently with systemic relapse. In extremely rare cases, the blast phase can affect the CNS without bone marrow involvement. Tyrosine kinase inhibitors (TKI) have become the treatment of choice for CML. However, there is poor penetration of CNS by some of these drugs or their active metabolites. Therefore, CNS may act as a sanctuary site for malignant cells in CML patients treated with TKIs. Here we describe an unusual case of CML who presented in accelerated-phase and multiple intracranial hemorrhages, and developed isolated CNS blast crisis after one year in spite of being in systemic remission.
Clinical presentation
A previously healthy 27-years-old male presented with10 days history of fatigue, abdominal pain and vomiting. He also complained of weight loss and low grade fever. Abdominal examination revealed huge splenomegaly. Investigations showed a white cell count of 538Í 109/l, hemoglobin 7.2 g/dl and platelets 47Í 109/l. Blood film showed marked leukocytosis with left shift, blasts 9% and thrombocytopenia, consistent with accelerated-phase CML. A bone marrow (BM) aspirate confirmed the above findings. Cytogenetic analysis of the bone marrow revealed100% Philadelphia chromosome and BCR/ABL positivity.
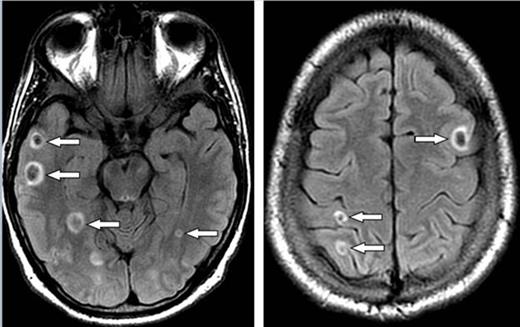
After admission, the patient developed headache and vomiting. MRI of brain showed multiple small hemorrhages in the supratentorial and infratentorial compartments (figure). The patient was diagnosed with accelerated-phase CML and leukostasis. Emergency leukapheresis was performed (two sessions) resulting in a decrease in his WBC count.
He was also started on hydroxurea, nilotinib and cytarabine 100mg, which led to improvement of his general condition and control of leukocyte count. He was continued on nilotinib 400 mg twice daily. He achieved complete molecular remission. Brain radiotherapy was considered because of brain hemorrhages and fear of lodging of blasts in the brain but not given because of opinion against it by expert colleagues. He was also referred for allogeneic stem-cell-transplant (SCT) because of the above concerns but not considered because of excellent response to nilotinib.
After 1year of initial diagnosis, he was readmitted with headache and bilateral visional loss. Fundoscopy showed retinal hemorrhages. His CBC, BM biopsy and brain MRI were normal. Lumbar puncture showed markedly increased CSF pressure (55cm) and leukocyte infiltration with many blast cells (42%).
Patient was diagnosed as CNS blast crisis of CML with BM in molecular remission. He was stareted on intrathecal chemotherapy (ITC), triple regime (methotrexate 6mg, ARA-C 30 mg, hydrocortisone 30 mg) and nilotinib was changed to dasatinib. His CSF cleared after multiple sessions of ITC; unfortunately, significant visual impairment persisted. Patient also received radiotherapy to the brain. He went on to have a sibling SCT and remains well 8 months post transplant.
Conclusion
We describe a young male with accelerated-phase CML and multiple brain hemorrhages on presentation and subsequent isolated CNS blast crisis. We speculate that there was a possible link between the initial brain hemorrhages causing lodging and proliferation of blasts in the brain and subsequent isolated CNS blast crisis. We suggest that treatment options in such cases should include consideration of cranial irradiation initially, a tyrosine kinase inhibitor with better CNS penetration like dasatinib, and upfront allogeneic SCT as potential therapeutic modalities.
MRI brain FLAIR images show multiple ring like foci of recent hemorrhages (arrows).
MRI brain FLAIR images show multiple ring like foci of recent hemorrhages (arrows).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal