Abstract
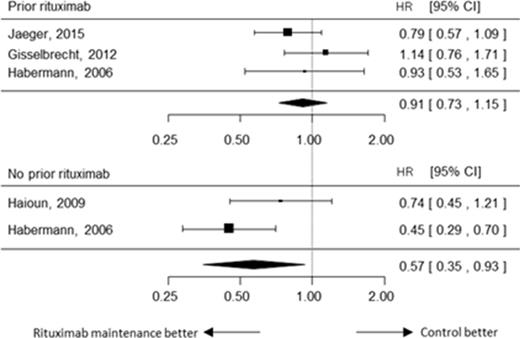
Whilst maintenance therapy with rituximab has been established its role as for follicular lymphoma with high tumor burden, its clinical relevance in aggressive lymphoma still remains to be elucidated due to controversial results of previous studies. In order to address this issue, we conducted a meta-analysis targeting CD20 positive diffuse large B cell lymphoma. We collected prospective randomized trials where case cohorts were administered with single agent rituximab as maintenance therapy for responding patients (PR or better) to induction treatments with or without consolidative autologous stem cell transplantation (ASCT), and were compared with control cohorts just followed with observation. Out of the 387 candidate reports, we extracted four relevant papers. Rituximab maintenance was placed as the first-line treatment scheme in three studies and second-line or later in one. The pooled estimates of the effect were calculated using random-effect model according to the method of Der Simonian-Laird with inverse variance weighting. Hazard ratio (HR) was selected as measures for responses, and risk difference (RD) for adverse effects. When HR was not available for a given study, it was estimated using methods described by Tierney et al. We assessed heterogeneity of the trial results using a chi-square test of heterogeneity and the I2 measure of inconsistency. Data of the 1546 patients of aggressive lymphoma from four studies comprising of 773 subjects each in maintenance and observation arms. Overall, rituximab maintenance had marginal impact on event-free survival (hazard ratio (HR): 0.80, 95% confidential interval (CI): 0.63 - 1.02, p=0.0719). Heterogeneity among all the trials was not statistically significant (p=0.19, I2=37.01%). To investigate the factors associated with significant impact of rituximab maintenance, we performed subset analyses according to various parameters inherent to study design of each report. No use of rituximab as part of induction treatment prior to randomization was significantly associated with better EFS in the rituximab maintenance arm (HR: 0.57, 95% CI: 0.35 - 0.93, p=0.024). By contrast, rituximab maintenance had almost no impact on outcomes when patients had already received rituximab before (HR: 0.91, 95%CI: 0.73 - 1.15, p=0.437). Furthermore, rituximab maintenance had positive effect when used in the first-line treatment scheme (HR: 0.72, 95% CI: 0.58 - 0.89, p=0.0026). When ASCT was not included in the treatments prior to randomization, rituximab maintenance significantly improved EFS (HR: 0.71, 95% CI: 0.56 - 0.91, p=0.0057). In order to examine relative impact of these parameters, we conducted meta-analyses using mixed-effects model treating these parameters (ASCT in prior treatment, rituximab in prior treatment, in first-line scheme) as categorical moderators. Prior rituximab administration before randomization was the sole significant factor (beta=0.6017, p=0.0253). Notably, in this model, residual heterogeneity disappeared almost completely (I2=0.0%, test for residual heterogeneity p=0.62), suggesting that the three parameters representing the difference of study design accounts for almost all of variety in effect-sizes among them. This suggests that rituximab included in induction therapy is sufficient to exert its role for responding aggressive lymphoma. Rituximab maintenance was associated with neutropenia (RD: 0.06, 95% CI: 0.01 - 0.12) and marginal increase of infection (RD: 0.14, 95% CI: -0.08 - 0.36). In conclusion, rituximab maintenance was not associated with better EFS in overall subjects. It has positive effect on EFS only when rituximab was not used in the induction therapy, which is a rare situation nowadays, negating practical usefulness of adding rituximab maintenance for aggressive lymphoma.
Tsurumi:Chugai Pharmaceuticals: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal