Abstract
Background: PTCL-NOS usually lacks B-cell associated antigens. However, rare cases of CD20 positive peripheral T cell lymphpoma have been reported[1-4], with the majority of cases being classified as PTCL-NOS[4]. So far, the vast majority of the published reports on CD20+ PTCL are from US or European countries with limited data on Chinese patients. Furthermore, the clinical and prognostic profile of this rare disease entity remains largely unknown.
Aim: To explore the clinical features and prognostic impact of aberrant CD20 expression in Chinese patients with PTCL-NOS.
Methods: We retrospectively reviewed patients diagnosed with PTCL-NOS at our institution from August 2002 to March 2015. Patients with aberrant expression of CD20 confirmed by immunohistochemical analyses were included in the study. We examined patients' pathological and clinical features, treatment response and survival.
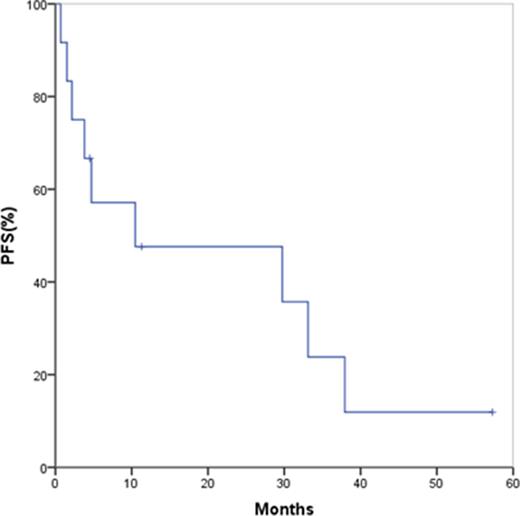
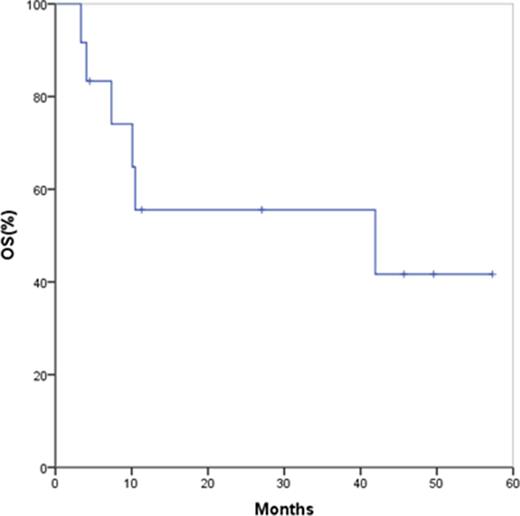
Results: Twelve patients with CD20+ PTCL-NOS were identified. CD20 was strongly and uniformly expressed in 6 cases and dimly expressed or present on a subgroup of neoplastic cells in the remaining cases. In 6 patients, the gene rearrangement studies for immunoglobulin and T-cell receptors were performed to determine the precise lineage for neoplastic clones. The Ki-67 proliferation index ranged from 10~85% in these cases. Among the patients, there were 10 men and 2 women. Patients' median age was 54 yr (range:16~69 yr). The majority(83%) of patients had a ECOG-PS score of 0~1. Eight (67%) patients presented with advanced stage (Ann Arbor stage 3~4) disease and the remaining 3 patients presented with localized (stage 1~2) disease. Nodal disease was present in all the patients, whereas 6 patients had extra-nodal involvement including the parotid glands, tongue, oropharynx, subcutaneous tissue, spleen, lung and breast. No patient presented with bone marrow involvement. The IPI score was 0~1 in 5 cases, 2 in one case, and 3~4 in 6 cases. All patients were initially treated with CHOP-like combination chemotherapy with a response rate of 75% (CR in 5 patients, PR in 4 patients, SD in 1 patient and PD in 2 patients). Three patients with stage 1~2 disease received consolidation radiotherapy, and no patient received autologous or allogeneic stem cell transplantation. Among CR patients, three remained disease-free at 4.5, 11.3 and 57 months, respectively. The remaining 9 patients developed disease recurrence or progression, among whom seven underwent gemcitabine-based salvage chemotherapy. No patient received rituximab in first-line or subsequent lines of treatment. At last follow-up, 6 patients have died from disease progression. The median PFS and OS for all the patients were 10.5 months (range:0.7~57 months, Figure 1) and 41.9 months (range:3.4~57 months, Figure 2), respectively.
Conclusions: CD20-expressing PTCL-NOS is rare, and appears to be clinically heterogeneous with a subset of patients associated with high IPI score and more aggressive clinical course. Despite the expression of B-cell antigens, the overall treatment outcome with anthracycline-based chemotherapy remains poor, and prognosis is similar to that of CD20 negative PTCL-NOS. The aberrant expression of CD20 may warrant further exploration of the role of rituximab in these patients. The clinical and prognostic implications of CD20 positivity in PTCL-NOS patients needs to be further elucidated in large-scale case series.
References:
[1] J Clin Oncol. 2011;29(32):e789-91.
[2] Case Rep Hematol. 2013:183134.
[3] Mod Pathol. 2001;14(2):105-10.
[4] Am J Surg Pathol. 2008;32(11):1593-607.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal