Abstract
Background: Acute erythroleukemia (AML-M6) is an aggressive myeloid leukemia, with poor outcomes (median survival < 12months). In 2008, the WHO further sub-classified this disease into two subgroups- erythroid leukemia and pure erythroid leukemia, based on the number of erythroblasts and myeloblasts. We carried out this study to evaluate differences in presenting features and outcomes between erythroid leukemia and pure erythroid leukemia.
Methods: After due IRB approval, out of 923 AML, 43(4.6%) pts who met the 2008 WHO criteria for acute erythroleukemia (2000-2014) were identified, and clinical characteristics retrospectively reviewed. A diagnosis of erythroid leukemia (M6a) was considered if > 50% of the total nucleate BM cells were of erythroid lineage and > 20% of non-erythroid cells were myeloblasts. Pure erythroid leukemia (M6b) was diagnosed in pts who presented with > 80% of BM nucleate cells consisting of immature erythroid precursors. Cytogenetic risk stratification was based on NCCN AML guidelines. Statistical comparisons were performed with the χ2 test for categorical variables and the Wilcoxon test for continuous variables. Univariate and multivariate analyses were performed with the Cox logistical regression. Survival analysis was based on the Kaplan-Meier method and log rank test. For all analyses, P ≤ 0.05 was considered statistically significant.
Results: The median age at diagnosis was 65 years (27-90) and 34(79%) were male. 30 (69%) had M6a and 13 (30%) had M6b. 27 (62%) had de novo AML M6, whereas 16 (37%) had secondary AML (9 underlying MDS and 7 therapy related).The median time to leukemic transformation for pts with underlying MDS was 8 months (2-83). Median follow up in our cohort was 7.2 months (2-157) at which time 13 (30%) deaths were documented.
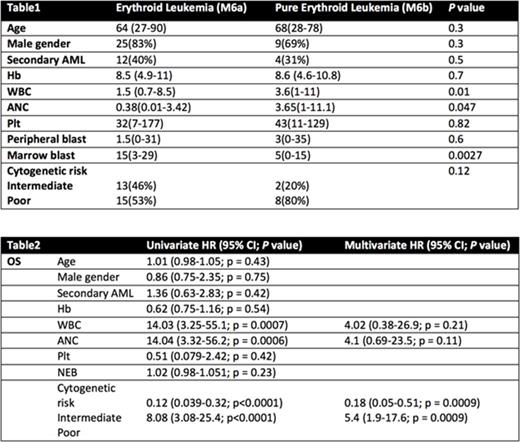
A. Patient characteristics: At time of diagnosis median laboratory values included; Hemoglobin 8.5 g/dL (4.6-11), WBC 2x109 (0.7-11.1), ANC 0.47x109 (0.01-4.07), Platelet 33x 109 (7-177), peripheral blast % 2 (0-35), and bone marrow blast % 11 (0-84). Cytogenetic information was available in 38 pts; of which 6(16%) were diploid, 21(55%) were complex/monosmal and 1(3%) was complex/non monosomal. Intermediate risk cytogenetic was observed in 15 pts (39%), and poor risk cytogenetic was identified in 23(61%). Comparing M6a and M6b, we observed that pts with M6a tend to have more leukopenia and neutropenia and higher marrow blast percentage compared to M6b (Table 1). None of the patients experienced extramedullary disease or CNS involvement.
B. Outcome and prognostics: We did observe a trend towards worse survival in pts with M6b, 7 months vs 12.9 months with M6a (p= 0.08) (Figure 1). There was no difference in survival in acute erythroleukemia compared to other acute myeloid leukemias, 10.1 vs 14 months (p= 0.28), respectively (Figure 2). In univariate analysis, WBC, ANC, and cytogenetic risk impacted survival (Table 2), however only cytogenetic risks retained significance in the multivariate model; Intermediate risk HR 0.18 (0.05-0.51; p = 0.0009) and poor risk HR 5.4 (1.9-17.6; p = 0.0009).
Conclusion: Acute Erythroid Leukemia is a rare leukemia with ~5% incidence in our cohort. We observed that regardless of the percentage of bone marrow erythroblasts and myeloblasts, survival in patients with Acute Erythroleukemia are predominantly impacted by cytogenetic risk stratification. This raises a question on the clinical relevance of the sub-categorization of acute erythroleukemia into erythroid leukemia and pure erythroid leukemia. Larger studies are needed to validate our results.
Al-Kali:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal