Abstract
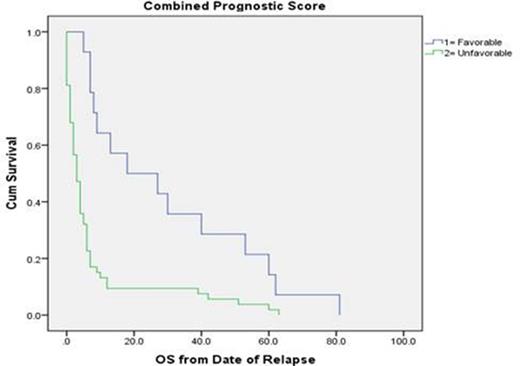
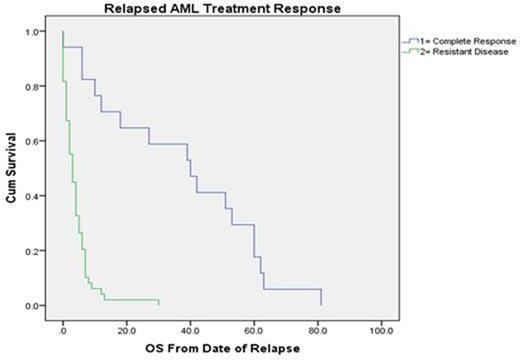
Introduction: Acute myeloid leukemia (AML) is one of the most lethal types of adult cancer, with 10,460 deaths among 18,860 diagnoses in 2014. Although some patients are cured with induction and consolidation chemotherapy with or without stem cell transplantation (SCT), between 50-80% of patients will either fail to obtain a complete remission (CR; primary refractory AML) or will relapse. The median overall survival (OS) for relapsed and refractory AML patients is dismal, and there is no clear consensus on the management of relapsed/refractory AML. In this study, with extended follow-up, we set out to look at our own experience with primary refractory and relapsed AML patients in order to try to identify the best therapy and factors associated with improved outcomes. Methods: This retrospective study in AML patients seen at Emory University Hospital (EUH) was IRB approved. Descriptive statistics were used to characterize the demographic and clinical variables. Cytogenetic and molecular signatures were defined based upon the European Leukemia Network and Southwest Oncology group classifications (Döhner et al. 2010, Slovak et al. 2000). Response criteria were based upon the revised recommendations of the International Working Group (Cheson et al. 2003). The combined prognostic score was created using previously validated prognostic variables including age (< 60 vs. >/= 60), Eastern Cooperative Oncology Group Performance Status (ECOG PS; 0-1 vs. >/= 2), and cytogenetic and molecular signatures (favorable vs unfavorable). A score of 0 was termed "favorable" and a score of 1 or greater was termed "unfavorable." The Kaplan-Meier and Cox proportional hazard statistical methods were used to estimate OS. Results: Review of electronic medical records identified 67 consecutive patients between January 1st 2008 and December 31st 2012 diagnosed with primary refractory or relapsed AML. Median age was 56 (range 18-81). Cytogenetic/molecular signatures were favorable in 6%, intermediate in 60%, and unfavorable in 34%, and PS was 0-1 in 34% and 2 in 66%. The majority of patients had a combined prognostic score of unfavorable (n = 53, 79%). Among the 67 patients, 17 (25%) achieved CR with salvage therapy, with 13 (76%) of those able to undergo SCT. With an extended follow-up of approximately 5.6 years, the median OS of our refractory/relapsed AML cohort was 4 months (95% CI 2.2-5.8), with 8% of patients living at least 5 years from their date of relapse. Univariate analysis identified the following factors to be associated with a significantly worse median OS: Secondary AML at initial diagnosis (2.0 vs 5.0 months; p = 0.005), unfavorable cytogenetic/molecular signature at initial diagnosis (3.0 vs 6.0 months; p = 0.014), ECOG PS of 2 or greater at relapse (2.0 vs. 7.0 months; p< 0.001), an unfavorable combined prognostic score at relapse (3.0 vs 18.0 months; p < 0.001), lack of SCT after salvage (3.0 vs. 39.0 months; p < 0.001), lack of treatment in the refractory/relapsed setting with the combination of induction chemotherapy and hypomethylating agents (1.0 vs 8.0 months; p < 0.001), and lack of attainment of CR in the refractory/relapsed setting (3.0 vs. 40.0 months; p < 0.001). In the final multivariable model, only a favorable combined prognostic score at relapse (hazard ratio, HR 0.5; 95% CI 0-0.8; p = 0.02; Figure 1) and ECOG PS of 0-1 (HR 0.42; 95% CI 0.1-0.8; p=0.04) were associated with an improved OS, while the lack of attainment of a CR in the refractory/relapsed setting (HR 15.9; 95%CI 15.2-16.6; p < 0.001; Figure 2) was associated with a worse OS. Conclusion: In our cohort, the median OS among all patients diagnosed with primary refractory/relapsed AML was dismal. Despite the incorporation of novel agents and treatment approaches among this vulnerable patient population, there remains significant heterogeneity in patient outcomes within the first year, with only a small minority having a significantly longer OS. Similarly to patients with newly diagnosed AML, the most important prognostic variables among our refractory/relapsed AML cohort appears to be their combined prognostic score and their ability to achieve a CR in the salvage setting. It may be beneficial for future studies to focus on improving both, modifiable patient prognostic factors (i.e., PS) and treatment approaches in order to achieve CR in the refractory/relapsed setting.
Kota:Pfizer: Membership on an entity's Board of Directors or advisory committees; Leukemia Lymphoma Society: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal