Abstract
Introduction: Erythropoietin resistant anemia persists for at least six months in patients discharged from intensive care unit (ICU) without any preexisting hematological disorders. Patients with greater than 10% total body surface area burn become anemic and are refractory to erythropoietin (Epo). Endogenous Epo is critical for the survival, proliferation and differentiation of erythroid progenitors during early-stage erythropoiesis. Erythropoiesis starts with the hematopoietic stem cell commitment to the erythroid lineage, and the newly developing erythroblasts are then nurtured in the erythroblastic islands (EBI), which support enucleating erythroblasts through adhesive interactions during terminal maturation. Our earlier reports in scald burn model indicate a myeloid bias following burn injury dictating bone marrow granulocyte monocyte progenitor versus megakaryocyte erythrocyte progenitors suggesting that Epo independent defects in CFU-E generation starts at the commitment stage. However, we found that Epo dependent proliferation remained intact in burn patient PBMC derived cultures, which was followed up to late erythroblast stage. Here we inquired whether erythroblast maturation stage is affected by burn injury, if so what phenotype of EBI macrophage contributes to the Epo resistant anemia in burn injury?
Methods: To this end, four patients (2F and 2M), 40±7 years of age and 49.9±6.6%, TBSA burn were studied with consent and IRB approval. Blood samples collected twice at 7-10 days and 29-31 days post burn were analyzed. Age matched healthy volunteers served as controls (C). RBCs were generated ex vivo from burn patients' peripheral blood mononuclear compartment (PBMC) derived multi potent progenitors (MPPs) cultured with growth factors and autologous plasma. As it is difficult to obtain bone marrow from burn patients, parallel investigations were done in our mouse model of scald burn (15% TBSA) which causes Epo resistant anemia. To this end, bilateral femurs were harvested on post burn days (PBD) 3, 7, 14, 21 and total bone marrow erythroblasts and macrophages were investigated for ER-HR3, Siglec-1 and Vcam-1 expression. Erythroblast phenotype was characterized by flow cytometry, and validated by a pathologist.
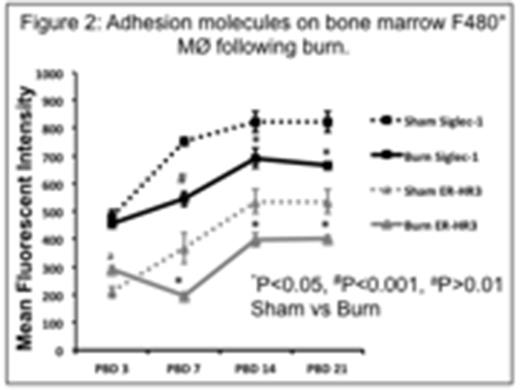
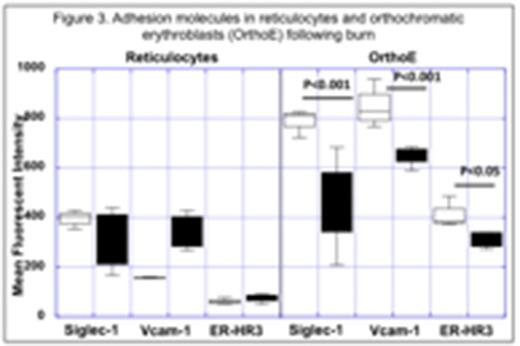
Results: We observed a defect in enucleation of orthochromatic erythroblasts (OrthoE) characterized by a significant 4-fold lower reticulocyte (CD235a+ CD71+/- Syto16-) to OrthoE (CD235a+ CD71+/- Syto16+) ratio (R/O) (P<0.05) post burn in patients compared to controls (Figure 1). In mice, peripheral hemoglobin, hematocrit and red blood cell counts were significantly lower from PBD 7 through PBD 21. In line with burn patient data, we observed similar impairment in enucleation of OrthoEs characterized by significantly lower reticulocyte (CD71+ Ter119+ Syto 16-) to OrthoE (CD71+ Ter119+ Syto 16+) ratio (R/O ratio) in the bone marrow of the burn versus control mice [2 fold lower R/O ratio from PBD 3 through PBD21 (P<0.05)]. We then investigated from both a macrophage and erythroblast perspective to understand the stage specific role of associated adhesion molecules. The mean fluorescence intensities (MFIs) of cell surface expressions of Siglec-1, and ER-HR3 were significantly decreased on F4/80+ macrophages from PBD 7 through PBD 21, (Figure 2) while changes in Vcam-1 was significantly low only on PBD 7. From the erythroblast perspective, only OrthoE expressed high intensities of macrophage adhesion molecules (Siglec1, Vcam-1 and ER-HR3) and not reticulocytes (Figure 3). However, the MFI of Siglec-1, Vcam-1 and ER-HR3 expression was significantly reduced on PBD 7, both in OrthoE and macrophages, indicating the essential role of these markers in enucleation.
Conclusion: Our data demonstrate defective erythroblast maturation following burn, and identify potential mediators of this process. These findings provide a framework for further investigations to determine the mechanistic basis of erythropoietin resistant anemia in burn patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal