Abstract
Background
Any inherited or acquired condition that increases the risk of developing deep venous thrombosis or pulmonary embolism is considered a thrombophilic disorder. Some examples of inherited causes of thromboembolic disorders are Factor V Leiden mutation (FVL), Prothrombin gene mutation, Protein C deficiency (low or dysfunctional), Protein S deficiency (low or dysfunctional), Anti-thrombin (AT) deficiency (low or dysfunctional). Use of these studies in clinical practice has been questioned. We attempted to identify if there are populations of patients that undergo more inpatient screening for inherited causes of venous thromboembolism (VTE).
Methods
Retrospective chart review of patients admitted with PE or DVT in a community teaching hospital between May 2012 and December 2014. Only patients who had DVT confirmed with ultrasound or PE confirmed with CT angiogram or had high probability of PE on V/Q scan were included in the study. Individual charts were reviewed to see if thrombophilia workup was ordered.
Results
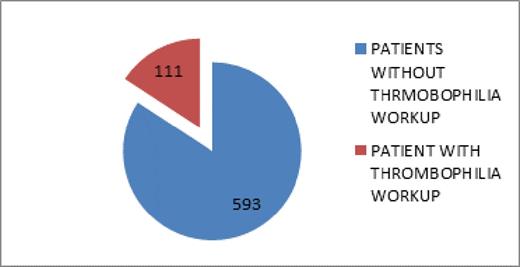
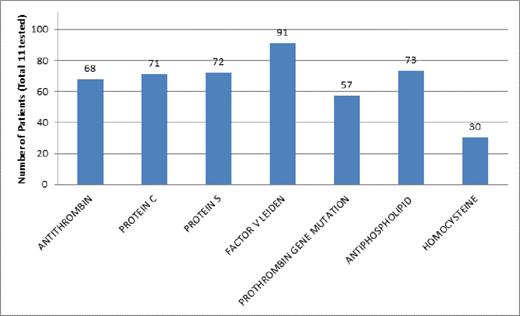
A total of 704 patients with acute venous thromboembolism were identified who met our inclusion criteria for the study. Of this 111 patients (15.76%) had one or more thrombophilia screening studies ordered. Risk factors related to venous thromboembolism were evaluated for all of the 704 patients. In our patient population, patients who were smokers (31% vs 20%), had history of sleep apnea (9% vs 3%), a past medical history (PMH) of VTE (37% vs 25%) or who had a family history (FH) of VTE (11% vs 4%) were more likely to have a thrombophilia workup ordered. Table 2 shows the frequency of individual thrombophilia studies ordered among the 111 patients who had testing performed and table 3 shows distribution of positive results.
| Test Result . | Abnormal Test Results . |
|---|---|
| ANA | 1 |
| Decreased AT III | 10 |
| Decreased Protein C | 10 |
| Decreased Protein S | 7 |
| Increased Homocysteine | 6 |
| Factor V Leiden | 4 |
| PT Gene Mutation | 1 |
| APLA | 1 |
| Test Result . | Abnormal Test Results . |
|---|---|
| ANA | 1 |
| Decreased AT III | 10 |
| Decreased Protein C | 10 |
| Decreased Protein S | 7 |
| Increased Homocysteine | 6 |
| Factor V Leiden | 4 |
| PT Gene Mutation | 1 |
| APLA | 1 |
Conclusion
The largest numbers of positive test results were noted for Protein C, Protein S and Antithrombin III and these are known to be affected by acute thrombosis and therefore could be false positives. Our study shows that those patients with PMH or FH of VTE were more likely to have thrombophilia studies. There is no consensus opinion as to whether to perform thrombophilia screenings in acute care settings. Given this and the fact that personal or family history of VTE do not usually modify future treatment decisions and that there may be significant number of false positives we do not recommend routine screening in these patient populations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal