Abstract
Background: The success of anti-cancer therapies continues to be threatened by formidable nosocomial infections caused by multi-drug resistant bacteria (MDR) which effectively "escape" the effects of anti-bacterial armory. The deluge of anti-bacterial resistance among gram positive and gram negative organisms poses a major challenge to all cancer care providers. The most concerning of MDR pathogens were first described by Rice and are known as the ESKAPE pathogens (Enterococcus fecalis, Methicillin resistant staphylococcus aureus, Klebsiella pneumonia, Aceinotobacter baumnii, Pseudomonas aerogenosa and enterobacter species) which represent the paradigms of pathogenesis, transmission and resistance. Herein, we present the epidemiology, risk factors and outcomes of ESKAPE infections in patients with hematological malignancies.
Methods: We conducted a retrospective review of clinical records of all patients with hematological malignancies seen at our institution. All episodes of infections with ESKAPE organisms were included. Data collected at baseline included demographics such as age, gender, comorbidities (DM/CHF/CKD/CLD), prior antibiotic therapy or hospitalization, use of empiric antibiotic therapy and presence or absence of catheter.
Results:
| . | AML . | ALL . | CLL . | CML . | MDS . |
|---|---|---|---|---|---|
| Age (Median) | 62 | 49 | 77 | 73 | 75 |
| Gender (M:F) | 1 | 1.05 | 1.07 | 0.62 | 0.78 |
| Type of ESKAPE (most common) | Staph | Staph | Staph | Staph | Staph |
| Median Length of stay (days) | 15 | 11 | 7 | 9 | 8 |
| All-cause mortality | 37.2% | 27% | 14.9% | 24.5% | 25.2% |
| . | AML . | ALL . | CLL . | CML . | MDS . |
|---|---|---|---|---|---|
| Age (Median) | 62 | 49 | 77 | 73 | 75 |
| Gender (M:F) | 1 | 1.05 | 1.07 | 0.62 | 0.78 |
| Type of ESKAPE (most common) | Staph | Staph | Staph | Staph | Staph |
| Median Length of stay (days) | 15 | 11 | 7 | 9 | 8 |
| All-cause mortality | 37.2% | 27% | 14.9% | 24.5% | 25.2% |
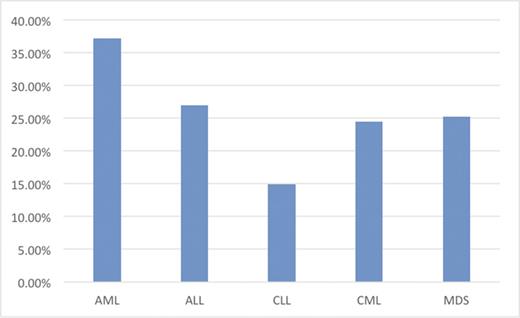
Baseline characteristics, most common type of ESKAPE organisms along with length of stay are summarized in Table 1. Most common underlying comorbidities noted were DM (4.8%), CKD (37.7%) and CHF (49.2%). The overall rate of septic shock was 20.7%. Of the 5585 patients with AML (13.8%), ALL (6.28%), CLL (6.94%), MDS (8.58%), 516 patients (9.23%) were noted to effected with ESKAPE organisms. All-cause mortality rates are shown in (Figure 1).
Discussion:
The impact of ESKAPE pathogens in hematological malignancies is still very limited with few studies so far and our retrospective analysis provides an account of ESKAPE infections in a large subset of patients with hematological malignancies. ESKAPE pathogens in our study accounted for 9.23% of infections. Despite a shift from Gram positive to Gram negative reported, our study showed a predominance of gram positive organisms. High rates of septic shock and early mortality are a growing concern with the ESKAPE bugs and all-cause mortality was shown to be significantly reduced by control of air quality, barrier isolation along with prophylactic use of antibiotics in a meta-analysis of infection control interventions among patients with acute leukemia and stem cell transplantation. Limited therapeutic options for ESKAPE pathogens along with a dearth of new effective drugs with novel mechanism of action calls for exigent therapeutic interventions to reduce their incidence. Cautious use of available antibiotics along with hand hygiene, screening of patients carrying resistant strains, isolation, decolonization and careful environmental cleaning should be emphasized to strategically control the ESKAPE bugs. Our study may be limited by residual confounding and institution specific variables given that it is a single center study and may not represent the general epidemiological patterns.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal