Abstract
Introduction: In published studies that included mostly hematopoietic cell transplants (HCTs) not using in vivo T cell depletion by ATG, there is a substantial survival difference between D-R- and D+R- patients, and a very small or no survival difference between D-R+ and D+R+ patients. We set out to determine the impact of donor CMV serostatus on survival after HCTs using ATG.
Methods: A total of 919 patients underwent myeloablative HCT for hematologic malignancies in Alberta between 1999 and 2014, with a uniform graft versus host disease (GVHD) prophylaxis using ATG (4.5 mg/kg given between day -2 and 0) in addition to methotrexate and cyclosporine. Monitoring for CMV reactivation was performed until at least day 100 after transplant using pp65 antigenemia (before 2008) or CMV DNAemia by quantitative polymerase chain reaction (since 2008). Preemptive therapy typically with ganciclovir was started whenever pp65 antigenemia exceeded 10 to 20 positive cells/200,000 granulocytes or CMV DNAemia exceeded 25,000 IU/mL plasma. Significance of survival difference between patient groups was tested using Cox proportional hazards analysis. Significance of difference in nonrelapse mortality (NRM) or cumulative incidence of relapse (CIR) was tested using Fine-Gray analysis (nonrelapse death was a competing risk of relapse and vice versa, in addition to graft failure and second malignancy). In all analyses, covariates included patient age (>45 vs ≤45), disease stage (acute leukemia in first remission, chronic myeloid leukemia in first chronic phase and myelodysplasia with <5% marrow blasts were considered good risk, all others poor risk), graft type (marrow vs PBSCs) and donor type (human leucocyte antigen [HLA] matched sibling vs other [typically matched unrelated]).
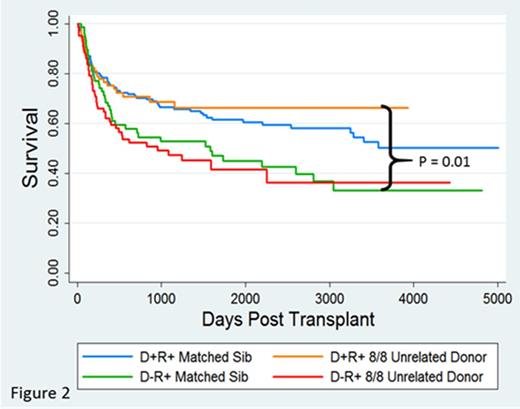
Results: D-R- and D+R- patients had similar survival (no significant difference) (blue vs orange curve, figure 1). D-R+ patients had a substantially lower survival than D+R+ patients with an estimated 5 year survival of 41% versus 60% respectively (Hazard Ratio [HR], 1.6; P = 0.001; 95% confidence interval[CI], 1.22-2.09) (red vs green curve, figure 1). This was due to higher NRM (sub hazard ratio [SHR], 1.76; P = 0.003; 95% CI, 1.212-2.58), not CIR. This appeared to be due to higher GVHD-associated mortality. We then compared D-R+ HLA matched sibling transplants with D+R+ HLA matched unrelated donor transplants to assess whether for a CMV seropositive patient with a CMV seronegative HLA matched sibling, search for a CMV seropositive HLA matched unrelated donor could be justified. D-R+ HLA matched sibling transplant recipients had a substantially lower survival than D+R+ 8/8 HLA allele matched unrelated donor transplant recipients with an estimated 5 year survival of 45% versus 66% respectively (HR, 1.7, P = 0.01, 95% CI, 1.10-2.89) (green vs orange curve, figure 2). This suggests that in the scenario of a seropositive patient with a seronegative matched sibling, unrelated donor search is justified.
Conclusion: Contrary to recommendations for HCTs not using ATG, choosing a seronegative donor for a seronegative patient is unimportant, whereas choosing a seropositive donor for a seropositive patient is very important (~20% absolute 5 year survival gain). Even if a seronegative HLA matched sibling donor is available for a seropositive patient, it is better to select a seropositive HLA matched unrelated donor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal