Abstract
Background
Optimization of pre-transplant risk assessment is a crucial issue to improve the allo-HSCT decision making process. Actually 3 major algorithms are in use in clinical practice: the EBMT risk score, the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) score and - more recently introduced - the refined Disease Risk Index (DRI).
DRI was defined to calibrate HSCT outcome across studies and centers. It was developed as a tool to assign patients into risk groups based on disease type and status at the time of transplantation. The aim of the DRI is to provide a robust tool that can be used for prognostication, for the analysis and interpretation of retrospective data, whether conducted in single-center, multicenter, or registry settings, or within the context of the federally mandated center outcome reporting. The DRI can also be used for the stratification of patients entering prospective HCT clinical trials.
DRI is not a fixed tool but instead it was conceived to be refined by the transplant community as new information becomes available.
Here we are presenting the results of a retrospective study designed to evaluate the 3 aforementioned score in stratification and prognostication of transplant outcome after a haploidentical HSCT (haplo-HSCT).
Patients and Methods
We included 220 adult patients (pts - 138 male, 82 female) who underwent a haplo-HSCT for hematologic malignancies, between 2006 and 2014 and were reported to our Institutional database. Risk assessment score and outcome analysis included all consecutive pts receiving an haplo-HSCT as 1st allogeneic transplantation. Pts receiving haplo-HSCT as 2nd or 3rd HSCT were excluded from the present analysis. Median age was 49 years (range, 15-77). The cohort included a broad representation of diseases (138/220 acute leukemia, 30 Hodgkin lymphoma); 62 pts were in complete remission at transplant, 158 were presenting active disease.
Conditioning regimens mostly rely upon the combination of treosulfan plus fludarabine (201/220) and total body irradiation (range 200 - 400 cGy) was utilized in 52 patients. GVHD prophylaxis consisted mostly of an mTor inhibitor (rapamycin) combined with mycophenolate mofetil. The majority of patients received peripheral blood stem cells from a family haploidentical donor as stem cell source, while only 4 patients received bone marrow transplant.
A written consent was given by pts allowing the use of medical records for research in accordance with the Declaration of Helsinki.
Results
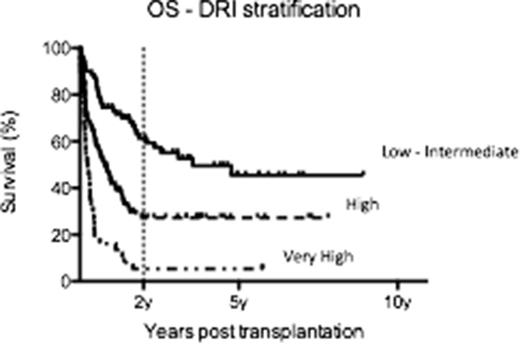
The median follow-up for survivors was 37 months (r 6-107). The overall survival (OS) at 2-y was 35% and the transplant related mortality at 100-days 23%. The 2y OS according to EBMT / HCT-CI / DRI risk score are reported in table 1.a and figure 1.
The evaluation of the HCT-CI impact after DRI stratification was able to show a significant difference in outcome showing better survival for pts with low DRI score and low HCT-CI score as expected (table 1.b).
Discussion
Refined DRI score and HCT-CI score predict survival after haplo-HSCT. The integrated application of refined DRI and HCT-CI may improve the definition of transplant eligibility for pts candidate to allogeneic HSCT form alternative donors including family haploidentical source.
| EBMT score . | 0-3 . | % pts . | 4-5 . | %pts . | > 5 . | %pts . | p . |
|---|---|---|---|---|---|---|---|
| 51% | 17 | 34% | 51 | 27% | 32 | 0.07 | |
| HCT-CI score | 0-2 | 3-4 | >/= 5 | ||||
| 48% | 59 | 36% | 31 | 0% | 10 | 0.0001 | |
| DRI score | Low-Intermediate | High | Very-High | ||||
| 61% | 32 | 27% | 51 | 5% | 17 | 0.0001 | |
| EBMT score . | 0-3 . | % pts . | 4-5 . | %pts . | > 5 . | %pts . | p . |
|---|---|---|---|---|---|---|---|
| 51% | 17 | 34% | 51 | 27% | 32 | 0.07 | |
| HCT-CI score | 0-2 | 3-4 | >/= 5 | ||||
| 48% | 59 | 36% | 31 | 0% | 10 | 0.0001 | |
| DRI score | Low-Intermediate | High | Very-High | ||||
| 61% | 32 | 27% | 51 | 5% | 17 | 0.0001 | |
| . | HCT-CI 0-4 . | HCT-CI >/=5 . | p . |
|---|---|---|---|
| DRI Low-Intermediate | 64% | 0% | 0.0001 |
| DRI High-Very High | 29% | 0% |
| . | HCT-CI 0-4 . | HCT-CI >/=5 . | p . |
|---|---|---|---|
| DRI Low-Intermediate | 64% | 0% | 0.0001 |
| DRI High-Very High | 29% | 0% |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal