Abstract
Patients with high-risk hematological malignancies have a poor prognosis without a hematopoietic stem cell transplant. An HLA- haploidentical donor is available in 95% of the cases, and post-transplant cyclophosphamide permits the use of T-cell replete grafts in settings were ex-vivo manipulation is not available. The experience with HLA-haploidentical HSCT with PBSC and post-tranplant Cy in the pediatric and adolescent population is limited; we report the following experience.
We retrospectively collected data on 25 patients (0 to 21 years old) with hematological malignancies, who underwent ambulatory haploidentical HSCT with post-transplant Cy from November 2011 to November 2014. The different conditioning regimens are described in Table 1. All patients received high-dose Cy(50mg/kg) on days +3 and +4. Cyclosporine A (CYA; 6mg/kg/d per os) and mycophenolate mofetil (MMF; 15mg/kg two times daily per os) were started on day +5. MMF was discontinued on day +35 and tapering of cyclosporin started day +90 in the absence of GVHD. All patients received anti-microbial prophylaxis for bacteria, fungal, herpes infection and Pneumocystis jiroveci according to institutional practices. First chimerism was performed at day +30, and second chimerism at day +100. Primary graft failure was defined when neutrophil counts did not exceed 0.5 x 109/L by day +30. Acute and chronic GVHD were graded according to NIH criteria.
Patient, donor and stem-cell harvest characteristics are described in Table 1. All patients had high risk hematological malignancies. There were 5 patients who underwent their first transplant on 1st CR, 4 with ALL with high risk cytogenetics and 1 with AML. All other patients were defined as high risk because they were refractory/relapsed.
Twenty-three patients (92%) had neutrophil engraftment after a median 17 (7-24) days. Platelet engraftment was observed in 20 (80%) patients after a median of 14.5 (11-23) days, 3 (12%) patients did not have platelet counts below 20,000/mcL. One patient was catalogued as a primary failure for not achieving neutrophil and platelet engraftment by day +30. One patient died before engraftment at day +10 of septic shock. Four patients (16%) died before day +30. The only patient that did not have a complete chimerism, had a diagnosis of AML and 30% of donor cells by day +30, by day +45 relapse of disease was documented.
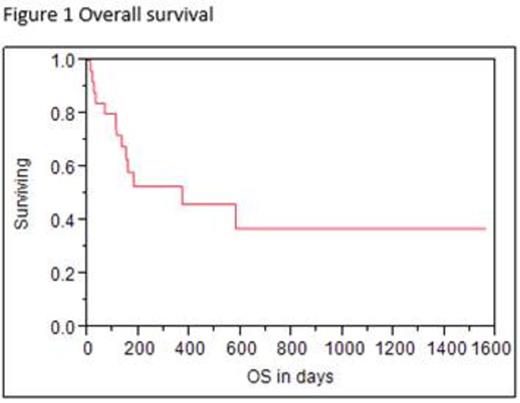
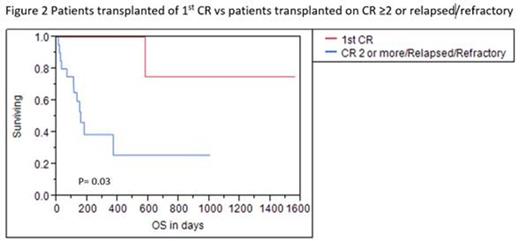
After a median follow-up of 157 days, 13 patients (52%) remain alive, with an estimated 1-year OS of 52% (95%CI: 30.4 - 65.6%).Nine patients (36%) died of complications (mainly infectious) not related to relapse at a median time of 66 days (10-579 days) from stem cell infusion. Nine patients (36%) relapsed in a median time of 105 days (45-288 days); three of those patients died at days +150, +113 and + 370 from transplant. Estimated 1 year event-free survival is 40.2% (95%CI: 41.3 - 75.8%) (Figures 1 and 2). Patients transplanted on 1st CR had a median follow-up of 664 days with an OS and EFS of 80% (4 patients), which was statistically different from the rest of the population (p=0.03) (Figure 3).
Among those who engrafted (n=21), 9 cases (42.9%) had grade 2-4 acute GVHD and 4 cases (19%) of grade 3-4 acute GVHD. Three patients (14.3%) developed chronic GVHD, two had mild skin or liver cGVHD. One patient had severe (NIH stage 3) skin cGVHD, she was alive and with a grade 2 cGVHD until last follow up at day +893.
Outpatient procedure, HLA-haploidentical HSCT including PBSC as a stem cell source, and post-transplant T-cell in vivo depletion using high-dose cyclophosphamide is feasible in children and adolescents, with acceptable rates of response and GVHD.
Patient, donor and harvest characteristics
| Variable . | N=25 . |
|---|---|
| Age, median(range in years) | 10 (1-21) |
| Gender, n(%) Male Female | 17 (68%) 8 (32%) |
| Diagnosis, n(%) ALL-B ALL-T AML CML | 16 (64%) 2 (8%) 5 (20%) 2 (8%) |
| Time from diagnosis to transplant (months) | 17.2 (1.9-153.5) |
| Conditioning regimen, n(%) Cy 1500mg/m2 + Flu 75mg/m2 + Bu 9.6mg/kg (IV) Cy 1050mg/m2 + Flu 75mg/m2 + Bu 12 mg/kg (oral) Cy/VP-16/RT Cy/Flu/Mel | 16 (64%) 6 (24%) 2 (8%) 1 (4%) |
| Donor, n(%) Mother Father Sister | 20 (80%) 3 (12%) 2 (8%) |
| Donor age, median(range in years) | 38 (17-49) |
| Infused CD34+ x 106/kg, median(range) | 11 (3.2-20) |
| Variable . | N=25 . |
|---|---|
| Age, median(range in years) | 10 (1-21) |
| Gender, n(%) Male Female | 17 (68%) 8 (32%) |
| Diagnosis, n(%) ALL-B ALL-T AML CML | 16 (64%) 2 (8%) 5 (20%) 2 (8%) |
| Time from diagnosis to transplant (months) | 17.2 (1.9-153.5) |
| Conditioning regimen, n(%) Cy 1500mg/m2 + Flu 75mg/m2 + Bu 9.6mg/kg (IV) Cy 1050mg/m2 + Flu 75mg/m2 + Bu 12 mg/kg (oral) Cy/VP-16/RT Cy/Flu/Mel | 16 (64%) 6 (24%) 2 (8%) 1 (4%) |
| Donor, n(%) Mother Father Sister | 20 (80%) 3 (12%) 2 (8%) |
| Donor age, median(range in years) | 38 (17-49) |
| Infused CD34+ x 106/kg, median(range) | 11 (3.2-20) |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal