Abstract
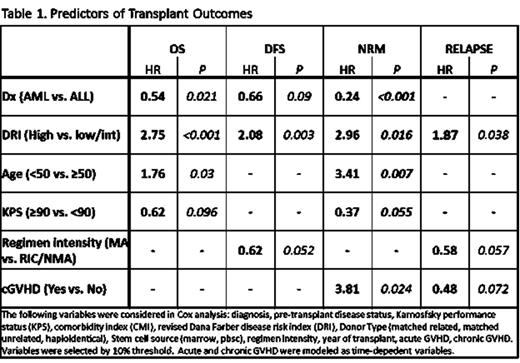
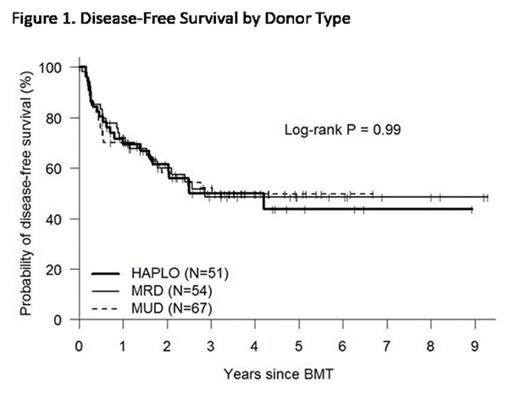
Allogeneic hematopoietic stem cell transplantation (HSCT) is considered the most potent post-remission antileukemic therapy in adults with acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL), although these benefits must be balanced by the increased morbidity and mortality associated with this procedure. We analyzed 172 consecutive acute leukemia patients transplanted in remission following a T cell-replete allogeneic HSCT from either a matched related, unrelated, or haploidentical marrow of PBSC donor, in order to look for patient-, disease-, and transplant-related factors associated with post-transplant outcomes. Patients were transplanted at a single institution between 3/15/06 to 12/19/14 and include 123 AML patients (CR1[94], CR2[28], CR3[1]) and 49 ALL patients (CR1[39], CR2[9], CR3[1]), median age 50 (range 19-74), median KPS 80 (70-90), median hematopoietic cell transplantation comorbidity index (HCT-CI) 2 (range 1-11), disease risk index (DRI) low, intermediate, and high in 5, 130, and 37 patients respectively per the revised Dana Farber/CIBMTR criteria. Transplant type was matched related donor (MRD), matched unrelated donor (MUD) and haploidentical (haplo) in 54 (31%), 67 (39%), and 51 (30%) patients respectively. Myeloablative chemotherapy was utilized in 122 (71%) patients, and PBSC was the source of stem cells in 142 (83%) patients. Compared to AML patients, ALL patients were more likely to be younger (median age 46 vs. 52, p=0.002) and had a trend for more myeloablative conditioning (82% vs. 67%, pp=0.063). Median f/u for surviving patients was 38 months. Acute GVHD grade II-IV occurred in 36% of patients, whereas chronic GVHD was seen in 46%. Estimated one year non-relapse mortality (NRM) at 1 and 3 years was 6% and 17% respectively. Three-year NRM was significantly higher for patients ≥50 years (24% vs. 10%) and for patients with ALL vs. AML (29% vs. 12%, p=0.022). The estimated 3 year OS, DFS, and relapse was 59%, 50%, and 33% respectively. Estimated 3-year OS was 70% for AML patients <50 years, compared with 59%, 58%, and 30% for AML ≥50, ALL <50, and ALL ≥50 respectively. In multivariate analysis, favorable risk factors for survival included a diagnosis of AML, non-high risk DRI, Age <50, and KPS ≥90 (Table 1). Myeloablative chemotherapy demonstrated a protective effect on relapse (HR 0.58, CI 0.37 - 0.93) and DFS (HR 0.62, CI 0.42 - 0.93), but was not a significant determinant of OS or NRM. Chronic GVHD had opposing effects on relapse (HR 0.48, CI 0.25 - 0.94) and NRM (HR 3.81, CI 1.44 - 10.1), with no impact on DFS or OS. Donor type (MRD, MUD, haploidentical) had no impact on any transplant outcome (figure 1). Following T cell-replete allogeneic HSCT for acute leukemia patients in remission, the primary determinants of success are type of leukemia, disease risk index, age, and performance status. Given the favorable outcomes associated with allogeneic HSCT in acute leukemia patients and lack of effect of donor type, we would argue that all patients with non-favorable risk acute leukemia should be offered an allogeneic HSCT as soon as any donor (MRD, MUD, or haploidentical) becomes available.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal