Abstract
Introduction: Acute myeloid leukemia (AML) patients failing to achieve complete remission or relapsing after intensive chemotherapy, have a dismal prognosis. In this setting, allogeneic hematopoietic cell transplantation (HCT) is a curative salvage therapy, but myeloablative conditioning (MAC) transplants are usually associated with high non-relapse mortality (NRM). Promising results have been reported using a sequential treatment approach (SEQ) consisting of cytoreductive chemotherapy, followed by reduced-intensity conditioning (RIC) and prophylactic transfusion of donor lymphocytes. Nevertheless, for young patients with refractory or relapsed AML, there is no definitive evidence to prefer SEQ rather than MAC HCT. The aim of this study, analysing the data from the SFGM-TC, was to compare the results of these two approaches in patients transplanted in AML not in complete remission.
Methods: Inclusion criteria: a) HCT performed from January 2006 to December 2013 b) Patient age up to 50 years (y), c) Transplant for refractory or relapsed AML, c) SEQ or MAC regimen d) Matched sibling donor, matched or mismatched unrelated donor.
PatientsÕ characteristics: 108 patients (median age: 38 y (range 1-50)) were analysed. Eighty-eight percent of patients were diagnosed with de novo AML and 12% with secondary AML. At diagnosis, 4% of patients were classified favorable, 33% Intermediate-1, 25% intermediate-2, and 38% adverse, according to the European LeukemiaNet (ELN) score. Before transplant, patients received a median of 2 lines of chemotherapy (range 0-3). At transplant, 53% of patients were in primary induction failure (PIF), 43% in relapse, and 4% were never treated and the median of bone marrow (BM) and circulating blast percentages were 19% (range 0-96) and 2% (range 0-93) respectively.
Transplant modalities: 60 patients received a SEQ approach (cytoreductive chemotherapy with FLAMSA (N=40) or with clofarabine (N=20) + high-dose cytarabine, followed by RIC combining cyclophosphamide (CY) with 4 Gy total body irradiation (TBI) or with busulfan (BU)) while 48 patients received a MAC regimen (CY combined with 10-12 Gy TBI (N=20) or with BU (N=28)). Forty-one percent of patients were transplanted from a sibling and 59% from an unrelated donor. Stem cell source was peripheral blood in 76% and BM in 24%.
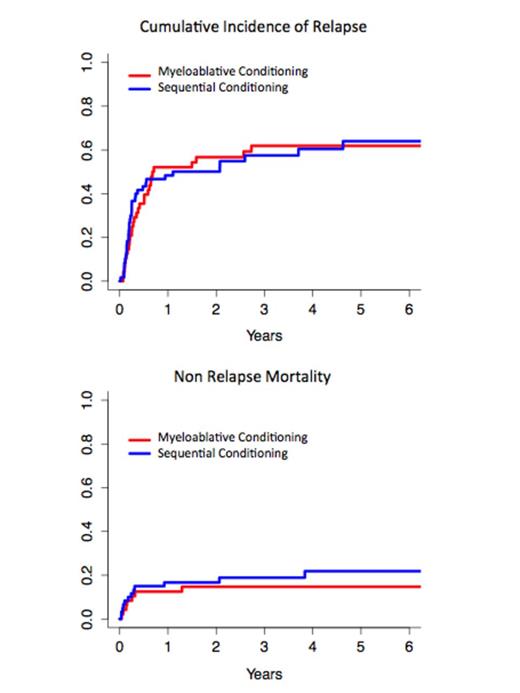
Results: MAC and SEQ groups had similar ages, ELN scores, numbers of pre-transplant chemotherapy lines and status at transplant. They only differed from the percentage of circulating blasts at transplant (median 1%, range (0-66) in MAC group vs 8%, range (0-93) in SEQ group, p=0.004) and from the time between diagnosis and transplant (median 164 days, range (62-610) and 239 days range (61-3702) respectively, p=0.036). In univariate analysis, type of conditioning regimen (MAC versus SEQ) did not impact post-transplant outcomes: 2-year overall survival (OS) was 37.2% (95% confidence interval (CI): 23.8-50.7%) in MAC patients vs 32.9% (95%CI: 21.4-44.9%) in SEQ patients (p=0.43); 2-year cumulative incidence of relapse was 56.7% (95%CI: 42.2-71.1%) vs 50.1% (95%CI: 37.2-63%) respectively (p=0.89) and 2-year non-relapse mortality was 14.7% (95%CI: 4.5-25%) vs 16.7% (95%CI: 7.1-26.2%) respectively (p=0.46). Grade II-IV acute graft versus host disease (GVHD) occurred more frequently in patients who received MAC: 66.7% vs 36.7% in the SEQ group (p=0.002), there was also a trend for more chronic-GVHD (41.7% vs 25%, p=0.066). Multivariate analysis identified high number of chemotherapy lines (hazard ratio (HR) 1.66, 95%CI 1.11-2, p=0.013) and high percentage of circulating blasts at transplant (HR 1.01, 95%CI 1.003-1, p=0.011), as factors independently associated with poor OS. Heterogeneity analyses performed for OS identified significant interactions between the type of HCT conditioning and BM blast percentage (p=0.01), or CD34+ cell dose (p=0,04), analysed as categorical variables with cut-offs at medians (20% and 6.106/kg, respectively). Though limited by low patients numbers, subgroup analyses suggested that SEQ HCT conferred a higher risk of death in patients with BM blasts > or = to 20% (HR=1.42), but a lower risk (HR=0.59) with BM blasts <20%, compared to MAC.
In conclusion, these data confirm that HCT is a valid salvage therapy for relapsed or refractory AML. In patients up to 50 years, both MAC and SEQ conditioning regimens offer similar outcomes, without increased NRM after MAC transplant.
Mohty:Janssen: Honoraria; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal