Abstract

Several scores have been developed, such as the Sorror index, which allow to identify before transplant subgroups of patients with different risks of death after allogeneic transplantation (AloTH). One of the parameters included in all these scores and routinely used in the pretransplant evaluation include cardiac function studies. However, it has been heterogeneously defined mainly based according to the ejection fraction using different approaches such as MUGA and echocardiography. The aim of our study was to evaluate the prognosis impact of pretransplant echocardiographic findings.
We retrospectively analyzed a total of 276 medical records of patients undergoing AloTH between 2006 and 2014. Additional data regarding demographic parameters, underlying disease, donor type, conditioning, engraftment, acute and chronic graft versus host disease, overall survival and cause of death were also included into the analysis.
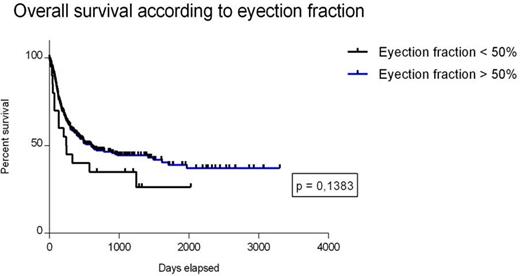
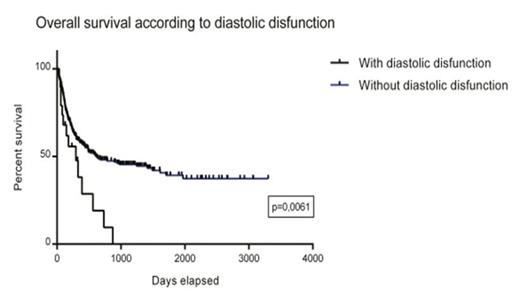
The mean ejection fraction was 61%, with 20 patients displaying an ejection fraction <50%. 19 patients (7%) had diastolic dysfunction, 5% valvular disease and 4% pericardial effusion. Of the 19 patients with diastolic dysfunction, 57% had been treated with anthracyclines: 7 patients (36%) were diagnosed with acute leukemia and 4 (21%)patients with lymphoma. In multivariate analysis we found that diastolic dysfunction was a predictor for survival (HR 5.43, 95% CI: 0,08-20,2, p = 0.028) and non-relapse mortality (HR = 5.7, 95% CI: 0,04-0,7, p = 0.002). Neither ejection fraction nor any other echocardiographic parameter predicted the risk of death.
In the present study pretransplant ejection fraction did not influence the prognosis of patients undergoing allogeneic transplantation; however, impaired diastolic function seems significantly influences post-transplant mortality. Therefore, in the pretransplant evaluation, diastolic function must be assessed in order to better define patient risks..
Falantes:Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal