Abstract

Introduction: The introduction of novel agentshas revolutionised the treatment of multiple myeloma, with improvements in survival of newly diagnosed and relapsed/refractory patients. However, despite these advances, the role for allogeneic haematopoietic stem cell transplantation (HSCT) in the treatment of these patients remains in question.
Reduced-intensity conditioning (RIC) HSCT with Seattle regimen (30 mg/m2 fludarabine and 2 Gray total-body irradiation, TBI) for multiple myeloma has been reported to be an effective treatment with low upfront toxicity, and the potential for graft-versus-myeloma effect (Niederwieser D et al, Blood, 2003). Its use as part of tandem HSCT (autologous HSCT followed by RIC-HSCT) is associated with a treatment-related mortality (TRM) rate as low as 15% (Björkstrand B et al, J Clin Onc, 2011). However, data on survival following auto-HSCT/RIC-HSCT is inconsistent and no unifying consensus has been reached regarding the optimal timing of RIC-HSCT in the treatment algorithm. In this retrospective multi-centre study, we investigated the safety, tolerability and efficacy of RIC-HSCT in multiple myeloma patients in remission following previous auto-HSCT.
Methods: A retrospective series was conducted for early-phase, high-risk myeloma patients who underwent RIC-HSCT following prior auto-HSCT in two tertiary transplant centres in Manchester in North West England, between November 2006 and July 2014.
Results: Over the eight-year period, 42 myeloma patients (male n=29, female n=13) underwent Seattle-conditioned RIC-HSCT following prior auto-HSCT. 66.6% (n=28) were performed in tandem. Median age at RIC-HSCT was 52 years (range 41-65), and median β2-microglobulin at diagnosis was 3.1 mg/L (range 1.6-18.0). 16 patients had cytogenetics assessed at the time of diagnosis, of which loss of TP53 and translocation of chromosome 14 were most common. 37 patients (88.1%) had previously been exposed to immunomodulatory agents (IMiDs). 53.3% patients (n=24) were in first remission at RIC-HSCT, whilst 37.8% (n=17) were in second remission. 31.1% (n=14) of RIC-HSCTs were performed after second auto-HSCT following previous relapse and re-induction chemotherapy. 34 patients (55.9%) had achieved at least a very good partial response (VGPR) prior to RIC-HSCT. RIC-HSCT was performed a median of 20 months (range 10-89) from diagnosis. Two patients (4.8%) required re-transplantation for failed engraftment, but subsequently engrafted following in vivo T cell-depleting regimens.
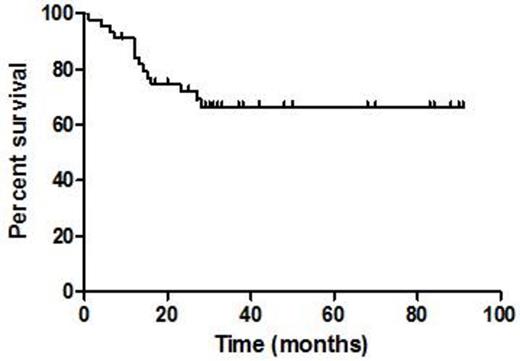
Mortality at early and interim time-points was low relative to registry and trial series, with TRM of 2.4% (n =1) and 9.5% (n=4) at day 100 and 365, respectively. 37 patients (82.2%) experienced chronic graft-versus-host disease (GVHD). Chronic skin GVHD was observed in 21 patients (grade 1-2: n=20; grade 3-4: n=1); chronic gastrointestinal GVHD in four patients (grade 1-2: n=1; grade 3-4: n=3); chronic hepatic GVHD in six patients (grade 1-2: n=4; grade 3-4: n=2); chronic oral GVHD in 17 patients (grade 1-2: n=17); and chronic ophthalmic GVHD in five patients (grade 1-2: n=5). There was an association between GVHD and enhanced disease control, as complete response rates increased from 26.5% to 51.5% by day 100 post-RIC-HSCT. However, 22 patients (48.9%) eventually relapsed with a median time to relapse of 6.5 months. 13 patients remain in CR one year post-RIC-HSCT. Relapse was treated with escalating donor lymphocyte infusions (DLI, n=13) or IMiDs (n=16). Response to lenalidomide at relapse was potentiated, despite the majority of patients having prior exposure to IMiDs. The median length of follow-up from diagnosis was 27 months (range 1-90). Median overall survival (OS) has not been reached; OS at two years was 69.2% (Figure 1).
Conclusions: In this retrospective series we demonstrate the feasibility of Seattle-conditioned RIC-HSCT in multiple myeloma. We observed a very low early TRM of 9.5% and presence of allo-immune disease control (graft-versus-myeloma effect), thereby augmenting IMiD efficacy. Chronic GVHD was prevalent and relapse occurred in a significant proportion of patients, but salvage with DLI and IMiDs highlighted the efficacy of the graft-versus-myeloma effect elicited by RIC-HSCT.
Survival outcomes after RIC-HSCT in myeloma. Median OS has not been reached, two-year OS was 69.2%.
Survival outcomes after RIC-HSCT in myeloma. Median OS has not been reached, two-year OS was 69.2%.
Cavet:Celgene: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Celgene: Other: Speaker. Tholouli:Pfizer: Honoraria, Speakers Bureau; MSD: Honoraria, Speakers Bureau; Jazz Pharmaceuticals: Honoraria, Speakers Bureau. Gibbs:Celgene: Honoraria; Takeda: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal