Abstract

Background
Ponatinib, a third generation TKI, induces high rates of cytogenetic and molecular responses in heavily pre-treated CML patients (pts) resistant to ≥2 TKI and/or with a T315I mutation, especially in CP (J. Cortes at al., NEJM 2013). This agent induces diverse non-severe adverse events (AEs), a substantial proportion of pts experience severe arterial thrombotic events [(ATE) 17% by 3 years, J. Cortes et al., Haematologica 2015]. This agent is now licensed and it is mandatory to explore the rates of responses and ATE in the real-life setting.
Aims
We took the opportunity of the French ponatinib compassionate use program between May 2013 (end of PACE inclusions) and January 2014 (ponatinib license) to evaluate different outcomes in real-life conditions.
Methods
This is a multicenter observational retrospective study, designed to examine safety and efficacy of ponatinib in CML (any phase) resistant/intolerant to prior TKIs, in university and non-university hospitals, benefiting from the national ponatinib compassionate use program. Data were captured and validated following the rules and regulations of observational studies in France. Pts were analyzed in intention-to-treat, Molecular biology tests were performed according to ELN guidelines and BCR-ABL/ABL are expressed as % IS in all centers. Standard clinical [gender, age, weight, body mass index (BMI), cardiovascular risk factors (previous events, tobacco abuse, high blood pressure, diabetes)], onset of any CV events before and during ponatinib treatment) and metabolic biological parameters (cholesterol, triglycerides) were collected.
Results
Thirty-five observations were collected in CP, 4 in AP and 5 in BC. We focused our analysis on the 35 CP pts only. There were 16 (46%) males and 19 females, with a median age of 53 (18-76) years at CML diagnosis and 59 (20-82) years at ponatinib initiation. Sokal scores were high in 13 (37%), intermediate in 12 (34%), low in 4 (12%) and unknown in 6 (17%); Euro scores were high in 6 (17%), intermediate in 15 (43%), low in 3 (9%) and unknown in 11 (31%); Eutos scores were high in 7 (20%), low in 20 (57%) and unknown in 8 (23%) pts. All pts harbored "major" BCR-ABL transcripts except one (e19a2). Regarding cardiovascular risk factors (CVRF) prior to ponatinib, 12 pts (34%) were treated for hypertension, 1 was diabetic, 6 (17%) had dyslipidemia (all on statins). Tobacco abuse was present in 8 (23%) pts and 14 pts had some pre-existing CVRF in total. Median weight just prior ponatinib was 66 (48-107) kg, and BMI was 24.2 (17.85-33) kg/m2. Thirteen (37%) pts were on anti-aggregants or anti-coagulants (AAG/C) prior to ponatinib. All pts had received imatinib first-line for a median of 29.5 (4-123) months, 20 (57%) dasatinib and 14 (40)% nilotinib as second-line, one pt developed a T315I after imatinib only; 21 (60%) had received all 3 TKIs prior to ponatinib.
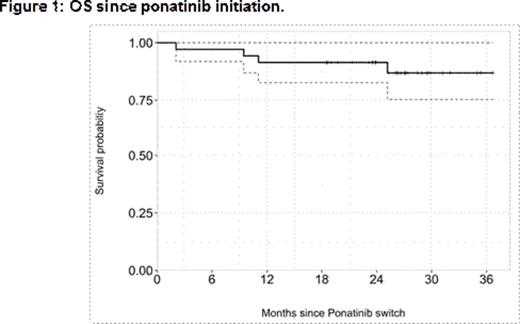
At ponatinib initiation, 7 (20%) harboured a T315I mutation, 7 (20%) other mutation(s) 20 (57%) none. In one case mutation screen was not performed. The trigger for ponatinib was resistance (hematologic, cytogenetic or molecular progression) in 26 (74%) pts, intolerance in 7 (20%) pts and both in 2 (6%) pts. Pts were initiated at a median of 45 (30-45) mg daily after a median of 79.5 (12-217) months of disease duration. The median follow-up on ponatinib was 26 (2-37) months. The cumulative incidence of major molecular responses was 29% at 3, 42% at 6, 56% at 12 and 70% at 18 months. The overall survival is shown in figure 1. Four pts died, 3 of disease progression and 1 of myocardial infarction.
Six (17%) pts had grade 3-4 hematologic AEs imposing transient ponatinib withhold, and 14 (40%) had diverse grade 1-2 non-hematologic, non-CV AEs (pancreatic, hepatic, skin toxicities, no grade 3-4). ATEs occurred in 19 (54%) pts after a median of 5.8 (0.7-21.7) months of ponatinib, without CVRF in 10 (53%) pts and without AAG/C in 13 (68%) pts. CVRF and AAG/C had no significant influence here on ATEs onset in univariate Cox model (p=0.76 and 0.37 respectively). Lipids and HbA1c were not modified on ponatinib. Overall 43% of pts stopped ponatinib for toxicity.
Conclusion
In the French compassionate use program in CP-CML patients resistant or intolerant to previous TKIs, ponatinib displayed strong efficacy, as previously described. In this unselected population of patients, ATEs were confirmed to represent the main tolerance concern in the real life setting.
Nicolini:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Ariad Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Coiteux:Novartis: Speakers Bureau; BMS: Speakers Bureau; ARIAD: Speakers Bureau. Charbonnier:Novartis: Speakers Bureau; BMS: Speakers Bureau; ARIAD: Speakers Bureau. Huguet:Novartis: Consultancy, Research Funding; PFIZER: Consultancy, Speakers Bureau; BMS: Consultancy, Speakers Bureau; ARIAD: Consultancy, Speakers Bureau. Etienne:ARIAD: Consultancy, Honoraria, Speakers Bureau; BMS: Consultancy, Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Other: Congress Travel/Accomodations, Research Funding, Speakers Bureau. Legros:Novartis: Research Funding, Speakers Bureau; ARIAD: Speakers Bureau; BMS: Speakers Bureau. Rousselot:Pfizer: Consultancy; BMS: Consultancy, Speakers Bureau; Novartis: Speakers Bureau. Amé:BMS: Speakers Bureau; Novartis: Speakers Bureau. DeFrance:Ariad: Consultancy. Mahon:ARIAD: Consultancy; Pfizer: Consultancy; Bristol-Myers Squibb: Consultancy, Honoraria; Novartis: Consultancy, Honoraria. Rea:Novartis: Honoraria; Bristol-Myers Squibb: Honoraria; Ariad: Honoraria; Pfizer: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal