Abstract
Background. Diffuse large B-cell lymphoma (DLBCL) is curable for the majority of patients treated with anthracycline based immunochemotherapy (IC). While most patients achieve response to initial therapy, a subset of patients are refractory to initial IC or become refractory to subsequent salvage therapies. Prognosis in this setting is very poor. Here we determine the incidence of refractory disease from a large cohort of DLBCL prospectively followed from diagnosis in the IC era and assess outcomes in these patients.
Methods. Patients were prospectively enrolled in the University of Iowa/Mayo Clinic Lymphoma SPORE Molecular Epidemiology Resource (MER) within 9 months of diagnosis. Patients were followed for relapse, retreatment, and death; all events were validated by medical record. This analysis includes patients with DLBCL or primary mediastinal B-cell lymphoma (PMBCL) who received initial treatment of anthracycline based immunochemotherapy; patients with primary CNS lymphoma or post-transplant lymphoproliferative disorders were excluded. Response to therapy was retrospectively classified per 2007 Revised Response Criteria for Malignant Lymphoma from available clinical and radiology records. Refractory disease was defined as having a best response to any systemic therapy of stable disease (SD), progressive disease (PD), or relapse within 12 months of autologous stem cell transplantation (SCT). We also examined patients with transient response to IC as defined by achieving an interim response (CR or PR) but having progressive disease at or prior to the end of the planned number of cycles of IC.
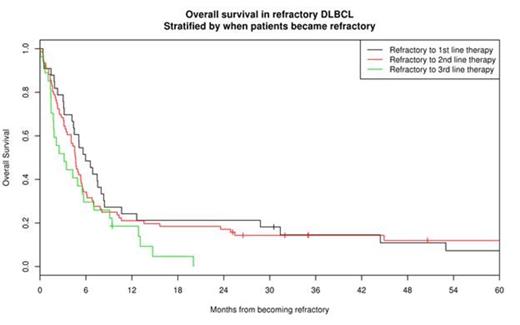
Results. 1039 patients with DLBCL or PMBCL lymphoma were enrolled in the MER from 2002-2012 and treated with R-CHOP or comparable IC. Median age at diagnosis was 62 years (range 18-91) and 577 (56%) were male. At a median FU of 60 months (range 1-148), 136 patients developed refractory disease. The median age at diagnosis of patients with refractory disease was 62 years (range 19-87). The cumulative incidence of refractory DLBCL was 11.3% at 2 years (95%: CI: 9.5-13.4) and 13.1% at 5 years (95% CI: 11.2-15.4). The median overall survival after becoming refractory was 4.7 months (95% CI: 4.1-5.5) with a 1 year survival rate of 21% (95% CI: 15%-30%).
The median number of therapies before becoming refractory was 2 with 35 patients becoming refractory following their first therapy (i.e. IC), 83 patients becoming refractory after their 2nd therapy, and 23 patients becoming refractory after their 3rd or later therapy; 27 patients had received stem cell transplant prior to becoming refractory. Outcomes were poor regardless of when patients became refractory (figure).
Patients received a median (range) of 2 (0-8) treatments after becoming refractory with 40% (N=54) attempting subsequent platinum based salvage therapy and 14% (N=9) proceeding to ASCT, of which only 6 remain alive in long-term remission. 41 patients (30%) were treated on clinical trials after becoming refractory. Response rate for the first therapy after becoming refractory was 21%, while 29% of patients had a response to any subsequent therapy. Once patients became refractory, there was no difference in survival based on response at end of initial IC (p=0.33), cell of origin at diagnosis (p=0.64), IPI at diagnosis (p=0.33), or age when refractory (p=0.66).
Outcomes in patients with transient response to IC (n=58) were poor, with the majority (N=37, 63%) becoming refractory to subsequent therapy. Median OS after first relapse was 6.7 months in patients with transient response to IC, which was equivalent to patients refractory to IC (p=0.99). The majority of patients with transient response to IC (69%) were next treated with platinum based salvage therapy which had a response rate of 40%. Ultimately 15 of the 58 patients (26%) proceeded to transplant, of which only 5 (9%) achieved long-term remission.
Conclusions. Approximately 13% of patients with DLBCL become refractory to treatment in their disease course. Outcomes once patients become refractory are extremely poor regardless of when patients become refractory. Standard prognostic factors are no longer predictive of outcome and stem cell transplant had limited benefit in this group of patients. Patients with transient response to initial immunochemotherapy should be included when classifying patients as refractory. New therapy strategies are needed in the refractory setting.
Maurer:Kite Pharma: Research Funding. Thompson:Kite Pharma: Research Funding. Farooq:Kite Pharma: Research Funding. Cerhan:Kite Pharma: Research Funding. Ansell:Bristol-Myers Squibb: Research Funding; Celldex: Research Funding. Link:Genentech: Consultancy, Research Funding; Kite Pharma: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal