Abstract
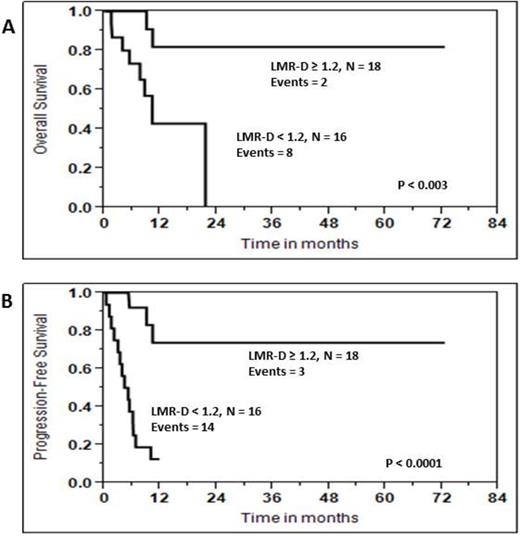
The lymphocyte-to-monocyte ratio at diagnosis (LMR-D) has been reported to be a prognostic factor for clinical outcomes in both T-cell and B-cell lymphomas. However, there are no reports testing the prognostic ability of LMR-D in patients diagnosed with de novo double/triple hit diffuse large B cell lymphoma (DLBCL). Thus, we set out to investigate if the LMR-D is a prognostic factor for survival in de novo double/triple hit lymphomas. From 10/5/1998 until 1/16/2015, thirty-four patients with de novo double/triple hit DLBCL were identified for this study. Double and triple hit were defined by interphase FISH evaluating three fusion signals to identify the BCL2 translocation and IGK/MYC D-FISH probe to identify whether the partner is IG or non-IG. Interphase fluorescence in situ hybridization (FISH) was performed on paraffin sections using probes that included 8q24 (5'MYC, 3'MYC); t (2;8), IGK/MYC; t(8,14), MYC/IGH; t(8;22), MYC/IGL; 3q27 (3'BCL6, 5'BCL'6); and 18q21 (3'BCL2, 5'BCL2). The cohort included 14 females and 20 males. The median follow-up for the cohort was 9.0 months (range: 0.4-72.6 months). Using the median for the LMR-D as the cut-off value, patients with a LMR-D ≥ 1.2 experienced superior overall survival (OS) [Hazard ratio (HR) of 0.127, 95% confidence interval (CI) of 0.019-0.530, p < 0.004] and progression-free survival (PFS) [HR of 0.107, 95 CI of 0.024-0.335, p < 0.0001]. The median follow up for OS for patients with a LMR-D ≥ 1.2 was not reached with a 5-year OS rate of 82% (95% CI of 49%-95%) compared with a median follow-up of 10 months for patients with a LMR-D < 1.2 with a 0% 5 year OS rate, p < 0.003 (Figure 1A). The median PFS for patients with a LMR-D ≥ 2 was not reached with a 5 years PFS of 74% (95%CI, of 43%-91%) compared with a median follow-up of 4.7 months for patients with a LMR-D < 1.2 and 0% 5 year PFS rate, p < 0.0001 (Figure 1B). After adjusting for the International Prognostic Index, multivariate analysis showed that the LMR-D remained an independent prognostic factor for OS [HR = 0.180, 95% CI of 0.254-0.784, p < 0.02] and for PFS [HR of 0.127, 95%CI of 0.029-0.409, p < 0.0003]. In spite of the small cohort of de novo double/triple hit DLBCL, the LMR-D was identified as a prognostic factor for clinical outcomes for this specific set of aggressive lymphomas. Further studies are warranted to confirm our findings.
| LMR-D ≥ 1.2, N = 18 Events = 2 . |
|---|
| LMR-D < 1.2, N = 16 Events = 8 |
| P < 0.003 |
| LMR-D ≥ 1.2, N = 18 Events = 3 |
| LMR-D < 1.2, N = 16 Events = 14 |
| P < 0.0001 |
| Figure 1 |
| A |
| B |
| LMR-D ≥ 1.2, N = 18 Events = 2 . |
|---|
| LMR-D < 1.2, N = 16 Events = 8 |
| P < 0.003 |
| LMR-D ≥ 1.2, N = 18 Events = 3 |
| LMR-D < 1.2, N = 16 Events = 14 |
| P < 0.0001 |
| Figure 1 |
| A |
| B |
Maurer:Kite Pharma: Research Funding. Ansell:Bristol-Myers Squibb: Research Funding; Celldex: Research Funding. Off Label Use: New agent in a combination regimen..
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal