Abstract
Blastic plasmacytoid dendritic cell neoplasm is a clonal disease derived from precursors of plasmacytoid dendritic cells (pDC). It is a rare neoplasm involving the skin which may or may not be associated from the outset with a leukemic component. The disease invariably progresses to aggressive leukemic dissemination, leading to a differential diagnosis with acute leukemia.
In 2004, we set up a French network to recruit biological data at diagnosis. Diagnosis was according to recommendations (Swerdlow et al, 2008), with, in addition, a mandatory panel of pDC markers (Garnache-Ottou et al, 2009) detected by flow cytometry or by immunohistochemistry on infiltrated blood, bone marrow or cutaneous lesions.
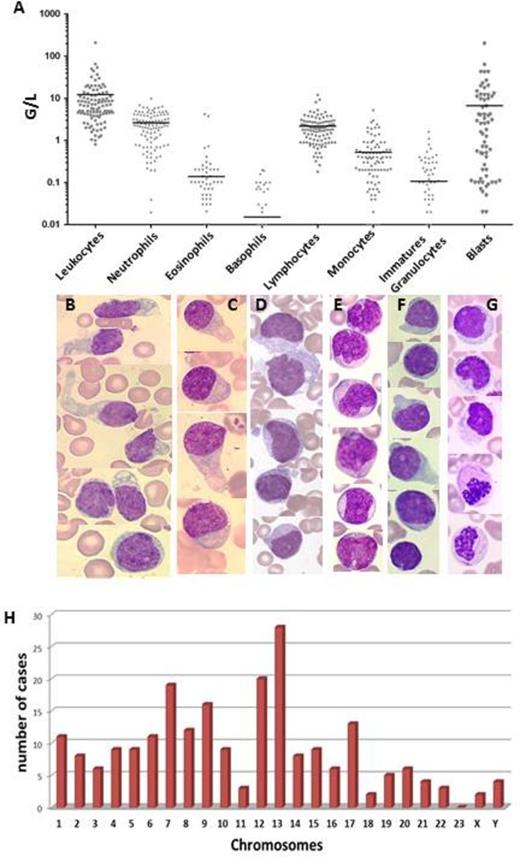
In total, 109 cases of BPDCN were included in 35 hospitals (2000-2013). BPDCN is more prevalent in men (sex ratio 4.4/1) and in elderly subjects (median age: 63 years; 7 patients were <20 yo).S kin lesions are very prevalent (85%) with variable lesion types. Blood cell counts show variable leukocytosis (figure 1A) with presence of blasts in 65% of cases. Anemia and thrombopenia were present in 59% and 76% of cases respectively. Bone marrow aspiration showed blastic infiltration in 94% of cases. Indeed, in 7 cases, there was isolated cutaneous involvement at diagnosis, with neither blood nor bone marrow infiltration. Morphologies of blast cells were heterogeneous. Typical morphologies were the most frequent, including medium-sized cells with a blastic round or irregular nucleus, cytoplasm displayed faint and irregular basophilia and no granulation. In a contingent of the blastic populations, we observed small vacuoles in a peculiar arrangement under the cytoplasmic membrane (42%) or the presence of large pseudopodia (28%) or both (17%) (Figure 1B, C, D). Some cases showed a more immature morphology with larger cells, higher nucleo-cytoplasmic ratio, very visible nucleoli and reinforced basophilia (28%) or a pseudomonoblastic morphology (5%) (Figure 1E). Rare cases presented a pseudolymphocytic form (7%, figure 1F) or large granulations in the cytoplasm (2%). Peroxidase and esterase were negative in all cases. Dysplasia of hematopoietic lineages was observed in 29% (figure 1G). For 8% of patients, myelodysplastic syndrome was diagnosed before the diagnosis of BPDCN.
Immunophenotype showed that HLA-DR and CD4 were expressed in all cases, but 4 cases did not express CD56 (confirmed using 3 different antibodies). Expression of markers of others hematopoietic lineages was frequent. Among myeloid markers, the most frequent was CD33 (46%), followed by CD117 (23%), whereas CD13, CD11c, CD15 and CD65 were rarely expressed. Monocyte markers (CD14, CD64, CD11b) and myeloperoxidase were never expressed. For the T lineage, CD2 and CD7 were the most frequent (62% and 58% respectively) whereas CD5 was rare (7%). No cytoplasmic or surface CD3 were detected. For the B lineage, CD22 was expressed in 16%, and low levels of cCD79a in 5%. Both were never expressed together, and no CD19, CD20 and immunoglobulins were found. Generally, we observed one of these antigens (Ags) per case, but in 44% of cases, there was a combination of 2 or 3 Ags from 2 or 3 different lineages. Immature Ags such as CD34 and CD133 were never found, and Tdt was found in 14% of cases.
Cytogenetic analysis revealed abnormal caryotype in 65% of the 78 caryotypes evaluated, with 20 cases having a complex caryotype. The frequency of the chromosomal abnormalities involved are shown in Figure 1H.
In conclusion, we describe the largest series of BPDCN to date in the literature. Detailed clinical and biological data at presentation allow improved recognition of this rare form of acute and aggressive leukemia, enabling early initiation of appropriate management.
A: Blood cell count in 109 BPDCN patients at diagnosis. Bars represent the median. B: Typical BPDCN morphology. C: In this case, the nuclei were peripheral, cytoplasm presented heterogenous basophilia, vacuoles were rare but large pseudopodia are frequent. D: Typical morphology with frequent microvacuoles under the cytoplasmic membrane. E: Immature morphology. F: Pseudolymphocytic morphology. G: Presence of dysplasia in myeloid cells with Auer Rods in the granulocytes. The morphology of the Blastic cells is typical. H. Chromosomal abnormalities in 78 caryotypes evaluated: The histogram represents the number of cases in which each chromosome was involved (deletion, gain, translocations).
A: Blood cell count in 109 BPDCN patients at diagnosis. Bars represent the median. B: Typical BPDCN morphology. C: In this case, the nuclei were peripheral, cytoplasm presented heterogenous basophilia, vacuoles were rare but large pseudopodia are frequent. D: Typical morphology with frequent microvacuoles under the cytoplasmic membrane. E: Immature morphology. F: Pseudolymphocytic morphology. G: Presence of dysplasia in myeloid cells with Auer Rods in the granulocytes. The morphology of the Blastic cells is typical. H. Chromosomal abnormalities in 78 caryotypes evaluated: The histogram represents the number of cases in which each chromosome was involved (deletion, gain, translocations).
Bardet:Celgene: Research Funding. Deconinck:CHUGAI: Other: Travel for international congress; PFIZER: Research Funding; ROCHE: Research Funding; NOVARTIS: Other: Travel for international congress; ALEXION: Other: Travel for international congress; JANSSEN: Other: Travel for international congress; LFB loboratory: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal