Abstract
Bone marrow biopsy (BMB) examination is an essential part of diagnosis for hematologic disorders. BMB length guidelines exist but are inconsistently followed; recommendations have included > 20mm for lymphoma (Cheson et al. JCO2014), 15 mm for myeloproliferative disease (Thiele et al. Haematologica 2005), 16 mm for malignant neoplasms in general (Bishop et al, J. Clin. Pathol. 1992). Poor BMB quality hinders pathology interpretation, may impact diagnosis, accurate lymphoma staging and may necessitate repeat procedure with associated patient anxiety and therapy delay. We had observed significant variation in BMB quality at our institution. We therefore undertook a quality improvement (QI) project to identify factors associated with suboptimal BMB and to implement strategies to improve overall BMB quality.
Aim: To evaluate the proportion of our biopsies that meet above criteria and identify factors that contribute to suboptimal sampling. The ultimate goal is to improve the quality and length of BMB at our institution for better diagnostic accuracy.
Methods: We collected data prospectively on 212 consecutive BMBs performed on adult patients at our institution for baseline evaluation. As BM performers knew about the project, we also collected retrospective data on BMB length to assess for a Hawthorne effect. We recorded the following BMB performance data: patient age, body mass index (BMI), clinic or inpatient setting, sedated or non-sedated procedure, needle gauge, use of trap, performing clinician and disease category. BMB performers included faculty, fellows and nurse practitioners. The BMB length, amount of marrow space, degree of crush and aspiration artifact and disease involvement were assessed in each case. We analyzed which BMB performance factors were associated with differences in BMB length and quality.
QI intervention: We performed an email survey on perceived BMB adequacy criteria, discussed overall results and coded individual performance data at a meeting of all providers. We also presented the guidelines about recommended BM length. Individual data were revealed confidentially to each performer.
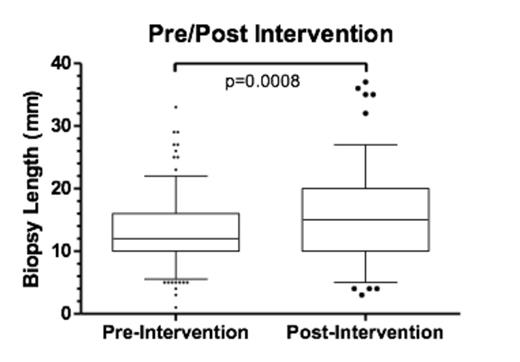
Follow up: Data on BM length and performer were collected on 122 BMB following the intervention. Two-tailed Student t tests under the normality assumption were used to determine significance of differences in BM lengths between pre and post intervention biopsies.
Results:
Baseline BMB: 210 BMB samples from 24 performers were evaluated. Results were compared to 104 historical marrows to rule out observation bias (Hawthorne effect). No difference was seen in biopsy lengths before or after initiation of study. Median biopsy length was 12 mm (range 1-35 mm). There were no statistically significant differences in BM length depending on patient BMI, location (inpatient vs outpatient), sedation, diagnosis and needle gauge. However there was significant variation in biopsy lengths between performers varying from a mean of 8 to 23 mm (p<0.001). This variation was not dependent on performer experience. The email survey showed that 7of 17 performers were unaware of 20mm recommended BM length for staging marrows, and 6 of 17 were unaware of 15 mm recommendation for other diagnoses. Shorter BMB was not limited to clinicians unaware of length recommendations; only 1 of 7 clinicians aware of staging length criteria achieved this consistently and 9 of 16 achieved criteria for other marrows.
Post QI intervention data: We evaluated a further 122 BMs from 15 performers. Median length increased from 12 mm to 15 mm (P<0.0001). This increase in BM length was attributable entirely to 3 performers whose BMs were significantly longer post intervention (p<0.05). Interestingly all these clinicians had been unaware of the BMB recommendations for staging and other BM samples prior to our discussion. Excluding these performers, there were no differences pre and post intervention.
Conclusions: BMB adequacy is highly dependent on the BMB performer. Other factors including BMI, disease, sedation and needle type do not significantly influence BM quality. Education on the value of adequate BM length and comparison between performers improves performance of some but not all clinicians. We plan to ask the clinicians whose BMB performance improved to discuss with our group to see if their experience can help others improve their BMB technique.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal