Abstract
Background: While most patients will not experience lasting neurocognitive effects from stem cell transplant, certain subgroups of patients may be particularly vulnerable to cognitive declines. The objective of this study was to identify factors that can predict the trajectory of neurocognitive functioning changes within the first six months after allogeneic hematopoietic stem cell transplantation (HCT).
Methods: Adult patient scheduled for their first allogeneic HCT completed a neuropsychological test battery to assess neurocognitive functioning prior to transplant, and at 100 days and six months post-transplant. The neuropsychological testing battery consisted of six tests over 3 domains: learning/memory, psychomotor efficiency/processing speed, and executive functioning/working memory. Sociodemographic (e.g. intelligence quotient (IQ), years of education) and transplant-related (e.g. conditioning regimen, HCT-Comorbidity Index) characteristics were collected at baseline. Additional clinical characteristics were collected at each time point, including Karnofsky Performance Status, acute graft-versus-host disease (GVHD) graded using revised Glucksberg grading system, chronic GVHD graded with National Institutes of Health consensus criteria, and patient-reported outcomes of fatigue, depressive symptoms, and physical symptom distress. Raw scores were converted to standardized T-scores (Mean=50, SD=10) based on demographically-adjusted norms. Neurocognitive impairment was defined as performance of <1.5 SD on two tests or <2 SD on one test. Composite scores for each domain were tabulated based on average of scores on constituent tests. Participants who completed the baseline and at least one follow-up visit were included in the analysis. Unconditional growth models were used to assess for overall changes in neurocognitive functioning over time. Multivariate multilevel models were then specified to identify predictors of the trajectory of neurocognitive functioning. To address the issue of missing data, a sensitivity analysis was conducted in which all models were replicated using only the data from complete cases, or participants who were assessed at every time point.
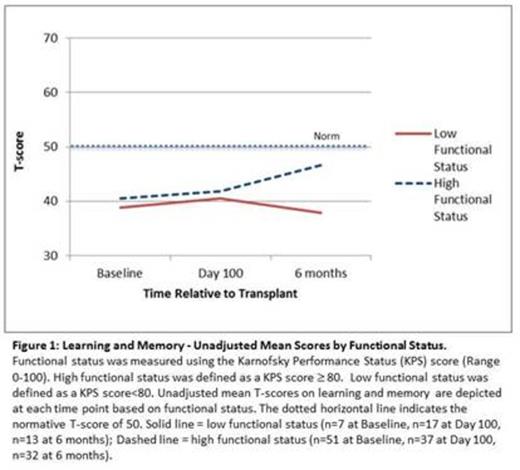
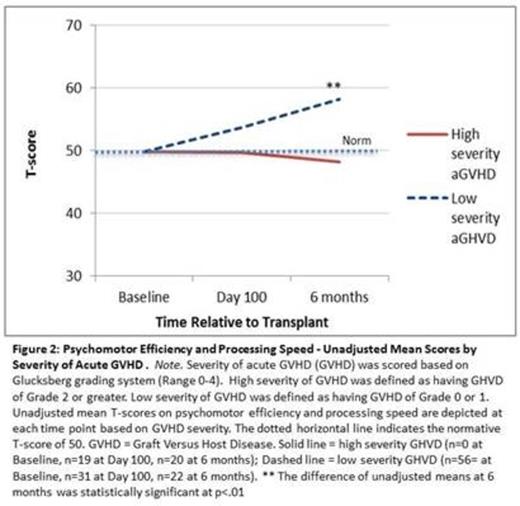
Results: 58 participants were included in the main analysis, 71% of whom provided data at all three time points. Missing data was mostly due to ill health preventing participation in study procedures. Mean age was 48.2 years; 47% were female; 81% of the sample was Caucasian. Mean years of formal education was 13.81 and the mean IQ was 114. The most frequent indications for allogeneic HCT included AML (34%), MDS (10%), CML (10%) and myelofibrosis (10%). 53% were treated with a myeloablative conditioning protocol. 46% of participants met the criteria for neuropsychological impairment prior to transplant. Mean T-scores of domain-specific neuropsychological performance prior to transplant were 39.93 (SD = 1.40) for learning/memory, 49.57 (SD = 1.26) for psychomotor efficiency/processing speed, and 49.37 (SD = 1.30) for executive functioning/working memory. Unconditional models specified overall improvements in learning/memory (3.64 units, p<.01), psychomotor efficiency/processing speed (3.44 units, p<.01), and executive functioning/working memory (3.82 units, p<.01) over the six months after transplant, that were not an effect of attrition. No significant change in the prevalence of overall impairment was detected over time. On multivariate analyses controlling for a range of sociodemographic and clinical predictors, Karnofsky Performance Status <80 was associated with worsening learning/memory over time (Figure 1); peak severity of acute GVHD higher than grade 2 was associated with worsening psychomotor efficiency/processing speed over time (Figure 2); and greater years of education predicted a faster improvement in psychomotor efficiency/processing speed over time. The effect of performance status and acute GVHD were maintained in subsequent sensitivity analyses.
Conclusions: Overall, domain-specific neuropsychological performance demonstrated mild but statistically significantly improvement over the first six months after transplant. However, post-transplant outcomes, such as low functional status and severe acute GVHD, may influence the direction of change in neurocognitive functioning.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal