Abstract
Introduction
Hepatic veno-occlusive disease (VOD), also known as sinusoidal obstruction syndrome (SOS) is a potentially fatal complication of HSCT and is characterized by hepatomegaly, right upper quadrant pain, jaundice, and ascites (Gratwohl A et al JAMA 2010). Severe VOD (sVOD) is clinically characterized by multi-organ dysfunction and is estimated to have a mortality rate of over 80% (Coppell JA et al BBMT 2010). VOD and particularly sVOD pose a significant economic burden in direct medical costs by adding an estimated $53,000 to HSCT (2004 U.S. dollars; Saito et al BBMT 2008), or $78,000 in 2015 dollars. However, little research has been conducted in ascertaining the indirect costs associated with premature death due to VOD. In our study, we developed an economic model to evaluate the indirect cost associated with premature death due to sVOD among HSCT patients in the U.S.
Methods
An Excel-based model was developed to estimate the indirect cost associated with premature death due to sVOD among HSCT patients. Model inputs included prevalence of sVOD as well as mortality, age, salary, employment rate, and life expectancy. Inputs were obtained from the published literature, Center for International Blood & Marrow Transplant Research (CIBMTR), Centers for Disease Control and Prevention (CDC), U.S. Census Bureau, and Organisation for Economic Co-operation and Development (OECD).
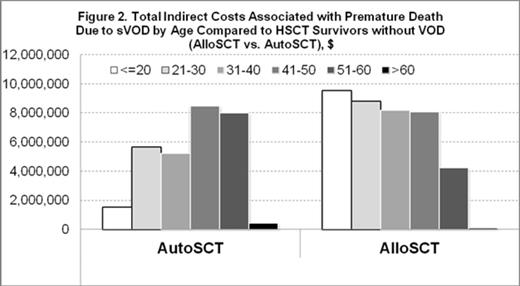
The model considered lost productivity as the result of premature death by calculating the number of years between the age of sVOD-related death and the assumed age of retirement (65 years old); it was assumed that the lifetime salary reflected underlying productivity of HSCT survivors who did not develop sVOD. Annual salary and life expectancy among HSCT survivors were adjusted from the general population to reflect decreased productivity in the first 2 years immediately following HSCT. Annual average salary inputs by age categories were assumed to be the same as the general population. Age of the working population was assumed to be between 18 and 65 years old.
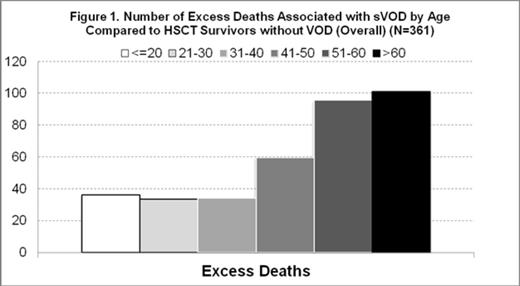
Excess mortality from sVOD was calculated as number of deaths among sVOD patients minus the number of deaths among HSCT patients who did not develop sVOD. Indirect cost was expressed as the cumulative salary for all productive years contributed by a patient and included a 3% discount for each additional year. Total lost productivity years and indirect costs by age category were obtained by multiplying each respective per patient value by the number of excess deaths in each age category. A sensitivity analysis was performed to examine the impact of changes in key model parameters on model results.
Results
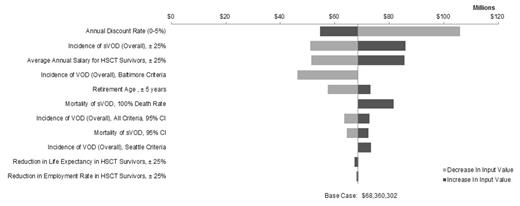
The model estimated 361 excess deaths per year due to sVOD in the HSCT population. The excess deaths due to sVOD were associated with indirect costs of over $68 million due to reduced life expectancy and consequent productivity loss. AlloSCT patients were younger on average, resulting in greater indirect costs ($39 million) compared to AutoSCT ($29 million). AlloSCT patients lost 3,637 productive years on average compared to 2,353 lost productive years for AutoSCT patients despite fewer patients receiving AlloSCT than AutoSCT. A sensitivity analysis showed that the total indirect costs due to overall VOD (non-severe and severe) were as high as $73.3 million.
Conclusion
sVOD imposes a substantial economic burden on patients in terms of excess deaths, lost productivity, and indirect costs. The model underestimates indirect costs largely due to not accounting for productivity loss among children and their caregivers or those older than 65. It also does not calculate productivity loss among HSCT survivors. Future research is warranted to elicit the additional indirect costs associated with non-severe VOD.
Deterministic Sensitivity Analysis: Total Indirect Costs due to Excess Deaths due to sVOD Compared with HSCT Survivors without VOD.
Deterministic Sensitivity Analysis: Total Indirect Costs due to Excess Deaths due to sVOD Compared with HSCT Survivors without VOD.
Quock:Jazz Pharmaceuticals: Employment, Equity Ownership. Zhou:Jazz Pharmaceuticals: Other: Analysis Group received funding for this analysis from Jazz Pharmaceuticals, Inc.; Analysis Group: Employment. Dai:Jazz Pharmaceuticals: Other: Analysis Group received funding for this analysis from Jazz Pharmaceuticals, Inc.; Analysis Group: Employment. Tang:Jazz Pharmaceuticals: Other: Analysis Group received funding for this analysis from Jazz Pharmaceuticals, Inc.; Analysis Group: Employment. Villa:Jazz Pharmaceuticals: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal