Abstract
Introduction: CB transplantation (CBT) after intermediate intensity conditioning is a less toxic alternative to CBT after high dose myeloablation. However, determinants of progression-free survival (PFS) and the impact of the pre-transplant revised Disease Risk Index (rDRI) and age-adjusted Hematopoietic Cell Transplant Co-morbidity Index (aaHCT-CI) are not established.
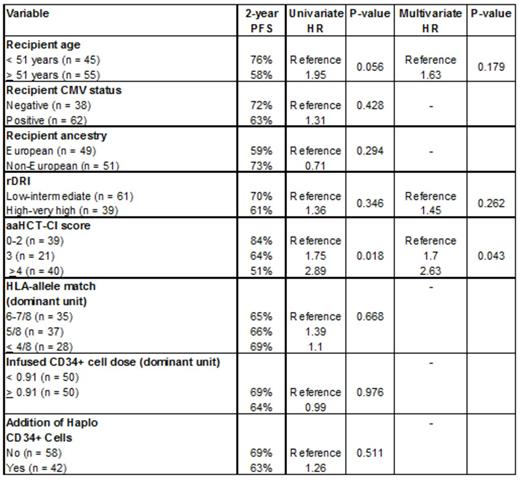
Methods: We evaluated 2-year PFS in double-unit CBT (dCBT) recipients with hematologic malignancies who were conditioned with a myeloablative but intermediate intensity regimen of cyclophosphamide 50 mg/kg, fludarabine 150 mg/m2, thiotepa 5-10 mg/kg, 400 cGy of TBI with cyclosporine-A/mycophenolate mofetil and no ATG. Eligible patients for this analysis included first allograft recipients aged < 70 years with acute leukemia, MDS, MPD (all < 10% blasts pre-transplant), B-cell NHL or HL. Patients were scored by the rDRI (with FLT-3 positivity categorized as high risk) and aaHCT-CI. PFS was estimated using the Kaplan-Meier method, while Cox proportional hazards regression models were used to assess the association between patient and graft characteristics and PFS.
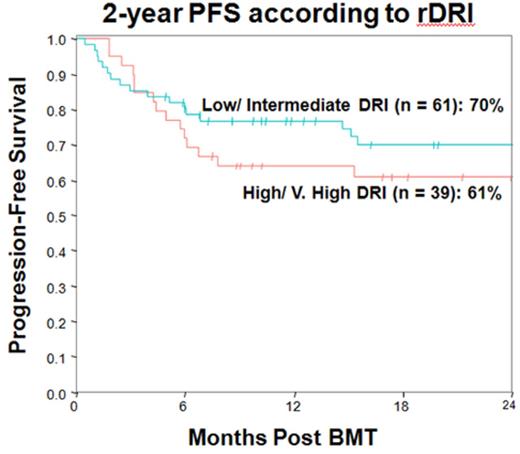
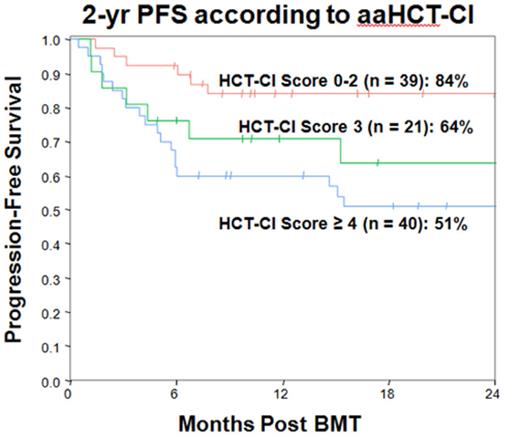
Results: Patients [n = 100, median age 51 years (range 19-70) and median weight 78 kg (32-139) had AML (38 CR1,17 CR2, 1 refractory), ALL (13 CR1, 2 CR2, 1 CR3), MDS (10, blasts ranging 1-10%), MPD (5), B-cell NHL (11 DLBCL or indolent) or HL (2). The rDRI distribution was 6 (6%) low, 55 (55%) intermediate, 34 (34%) high, and 5 (5%) very high whereas the median aaHCT-CI was 3 (range 0-9). The median infused CD34+ cell doses of the larger and smaller units were 1.17 (range 0.35-3.72) and 0.68 (range 0.17-2.18) x 105/kg, respectively, whereas the median 8 allele HLA-match was 5/8 (range 2-8/8). In 42/100 (42%) patients the dCBT grafts were supplemented by CD34+ cell selected haplo-identical peripheral blood stem cells. The cumulative incidence of day 45 neutrophil engraftment was 97% whereas day 100 grade II-IV and III-IV aGVHD were 69% and 15%, respectively, and 1-year chronic GVHD was 6%. Day 180 TRM was 17% and 2-year relapse incidence was 11%. With a median survivor follow-up of 27 months (range 5-91), the 2-year PFS was 66% (95%CI: 56-75). Kaplan-Meier estimates and univariate and multivariate analyses of 2-year PFS by relevant patient and graft variables are shown (Table and Figures). Dividing patients into low-intermediate vs high-very-high rDRI and aaHCT-CI 0-2, 3 and > 4 revealed high aaHCT-CI was associated with worse PFS whereas older age alone and high-very high rDRI were not. The adverse effect of high aaHCT-CI was mediated by an increased risk of TRM early post-transplant.
Conclusions: dCBT with intermediate intensity conditioning (Cy/Flu/Thio/TBI 400) is effective in adult patients with high-risk malignancies. Notably, pre-transplant rDRI was not associated with PFS suggesting this therapy is associated with a robust graft-versus-malignancy effect. High aaHCT-CI, however, adversely impacted PFS. These findings support the use of intermediate intensity dCBT in patients with high risk disease without concurrent high aaHCT-CI, and, as with adult donor allografts, new treatment strategies are required for patients with a significant co-morbidity burden.
Giralt:JAZZ: Consultancy, Honoraria, Research Funding, Speakers Bureau; TAKEDA: Consultancy, Honoraria, Research Funding; CELGENE: Consultancy, Honoraria, Research Funding; AMGEN: Consultancy, Research Funding; SANOFI: Consultancy, Honoraria, Research Funding. Scaradavou:National Cord Blood Program- New York Blood Center: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal