Abstract

Background:
High-dose therapy with autologous hematopoietic cell transplantation (autoHCT) is now well established as an effective therapy for lymphoma. However, infection is a known risk of autoHCT. Following autoHCT, prolonged lymphopenia (PL) and hypogammaglobulinemia (HypoGG) can occur and lead to a significant acquired immunodeficiency. While early recovery of lymphocyte count has been found to be a predictor of overall survival post autoHCT, the risk factors for and effects of PL and HypoGG in this population have not been carefully studied.
Methods:
We retrospectively reviewed all lymphoma patients who received their first autoHCT at the Medical College of Wisconsin from January 2009-December 2013. Patient charts were abstracted for pre-transplant disease characteristics (including lines of chemotherapy and regimens received prior to HCT, rituximab use, absolute lymphocyte count (ALC) pre-HCT, CD34+ and lymphocytes infused with HCT product) and post-transplant outcomes including day 100 ALC, 1 year IgG/A/M levels, and serious infections (SI). SI was defined as bacteremia, pneumonia, meningitis, pneumonia, clostridium difficile, neutropenic fever; or any infection requiring admission; or 2 or more infections of any type.
Primary outcomes of interest included whether SI correlated with Day 100 ALC and 1 year IgG/A/M levels. Survival outcomes (time to SI) were estimated using Kaplan Meier method, and comparisons made with Fisher's exact test, Chi-square tests, and log rank test. Multivariable analysis (MVA) was performed using the Cox proportional hazard regression. P-values of less than 0.05 were considered significant.
Results:
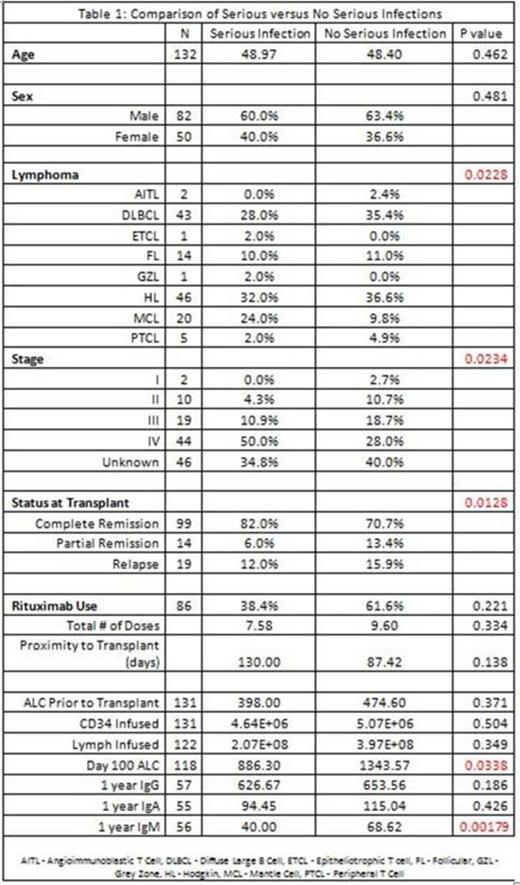
A total of 161 patients were included, of which 29 patients were excluded due to early relapse. Of the remaining 132 patients, 50 developed SI. Comparing the two groups (Table 1 - SI vs no SI), the majority of patients in both groups were Hodgkin Lymphoma, DLBCL, MCL, and FL with advanced stages at diagnosis. Prior to transplant, patients underwent >2 lines of chemotherapy and the majority were in complete remission at the time of transplant. Patients treated with HyperCVAD had a higher rate of SI (p<0.01) and ABVD had lower SI rate (p<0.01). 86 patients were treated with rituximab, with no difference in SI for total doses received or proximity to transplant. There was no association of ALC prior to transplant, CD34 infused, or lymphocytes infused with SI.
Post-transplant, patients with low day 100 ALC (p=0.04) and low 1 year IgM (p<0.01) had significantly higher rates of SI. This difference was retained on multivariate analysis. Interestingly, IgG level at 1 year did not predict for SI.
Conclusion:
We conclude that, following autoHCT, lymphoma patients with a day 100 ALC < 1200 or 1 year IgM < 60 are at significantly higher risk for SI. Contrary to our original hypothesis, day 100 ALC didnot correlate with 1 year Ig G/A/M levels. Other cell types, such as helper T cells and regulatory T cells, may also contribute to effective reconstitution of humoral immunity, such that ALC alone may not be a reliable predictor of immunoglobulin recovery.
Further prospective studies looking at subsets of lymphocytes, including B cells, T cell subsets, and NK cells may be helpful in identifying patients at significant risk for serious infections post autoHCT.
Hamadani:Celgene: Consultancy; Takeda: Research Funding; MedImmune: Consultancy; Cellerant: Consultancy. Hari:Janssen: Consultancy; Novartis: Consultancy; Spectrum: Consultancy; Sanofi: Consultancy; Takeda: Consultancy; Celgene: Consultancy; BMS: Consultancy. Fenske:Celgene: Honoraria; Seattle Genetics: Honoraria; Millennium/Takeda: Research Funding; Pharmacyclics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal