Abstract
BACKGROUND:
GVHD is a common complication of allogeneic hematopoietic stem cell transplantation (HSCT) leading to significant morbidity and mortality. Diagnosis of GI GVHD is difficult because there is no pathognomonic clinical manifestation or histologic feature. In an effort to better assess this complex clinical condition, we undertook a retrospective single center study to correlate histological data with clinical outcomes in patients (pts) with clinically suspected lower GI GVHD.
MATERIAL AND METHODS:
Three skilled pathologists of our center reviewed independently and retrospectively histological analysis of lower GI tract biopsies of all adult pts who have had a rectosigmoidoscopy or colonoscopy between January 1st, 2009 and December 31st, 2013, for a suspicion of lower GI GVHD (diarrhoea with or without abdominal pain after HSCT or DLI), whether they had received steroid treatment or not. Samples were scored according to the recommendations of the National Institutes of Health Consensus Project: 0 (no GVHD), 1 (possible GVHD: isolated and rare apoptotic bodies in epithelial cells associated with other possible explanation for histologic findings), 2 (probable GVHD: moderate apoptotic epithelial cells with no alternative explanation) and 3 (unequivocal evidence of GVHD). After this review, we analysed the correlation of each histological score (HS) with clinical features (intestinal stage 1 to 4 using the classic Glucksberg grading system) and biological data of pts at the time of endoscopy.
RESULTS:
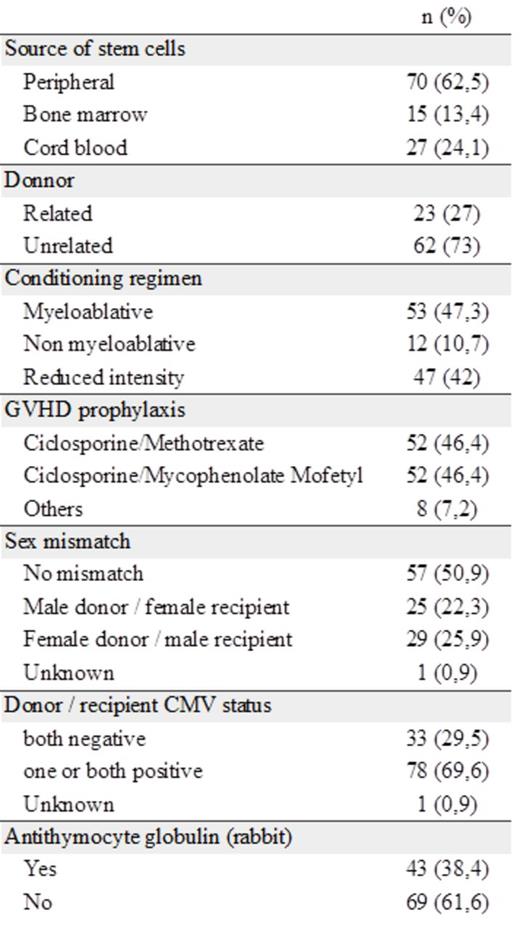
Hundred and twelve pts (74 men and 38 women) with a median age of 49 years (18-67) at transplant were included. The endoscopy was performed at a median time of 40.5 days after HSCT or DLI. The characteristics of pts at transplant are presented in Table 1.
HS of 0, 1, 2, 3 were attributed to 33 (29%), 21 (19%), 18 (16%) and 40 (36%) pts, respectively. Pts with HS of 0/1 had an intestinal stage of 1/2 in 57.5% of cases (n=31) and 3/4 in 42.5% (n=23). Pts with HS of 2/3 had an intestinal stage of 1/2 in 34.5% of cases (n=20) and 3/4 in 65.5% (n=38) (p=0.015).
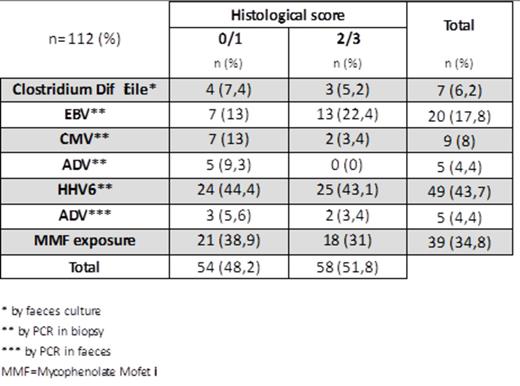
The incidence of co infections and other parameters which can disturb histological analysis is reported in Table 2. In particular, we report the presence of HHV6 in 49 patients (43.75%), and 13% of patients with HS 0/1 and intestinal stage 3/4 had a proven Clostridium Difficile colitis. We had only one sample of biopsy for 24 pts (21.4%).
Twenty-four pts of those with HS 0/1 (44.4%) died vs 38 of those with HS 2/3 (65.5%), and NRM was respectively of 11 (20.4%) vs 23 (39.6%).
With a median follow up of 49 months (20-77), the 3-y OS in groups with HS of 0/1 vs 2/3 was 59% vs 38%, respectively (p=0.02).
CONCLUSION:
Our study reports, in a large cohort of pts with clinically suspected lower GI GVHD, a good correlation between the lower intestinal histological scoring (reviewed by 3 independent pathologists) and clinical features, but not systematically. We have noted a high incidence of co viral or bacterial infections, and sometimes some difficulties to analyse the poor samples. This study strongly supports the value of a rigorous histological analysis in the diagnostic work-up of pts with suspected lower GI GVHD, because of its potential differential diagnoses, its risk of long exposure to steroid therapy, and its prognostic impact.
Characteristics of pts at transplant
Incidence of different biological and clinical parameters in each histological groups
Incidence of different biological and clinical parameters in each histological groups
Milpied:Celgene: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal