Abstract
Background: Although peripheral blood CD34+ stem cell counts by flow cytometry correlate well with yields, the time, complexity, and cost associated with flow cytometry limits its utility. Rapid, cost-effective, surrogate predictors (with <1hr turnaround) would allow for same-visit analyses and alteration of collection and mobilization strategies, particularly for the optimal use of time-sensitive and costly agents such as plerixafor. We previously demonstrated that morphologic parameters of neutrophil-like cells measured by hematology analyzers correlated with CD34 counts. We aimed to improve these models by using multiple regression analyses on data from a common hematology analyzer.
Methods: Patients undergoing stem cell apheresis were evaluated over a 6 month period. The day prior to initiation of apheresis, and on the morning of initial collection, peripheral blood samples were drawn into EDTA collection tubes and flow cytometric CD34 measurement and/or CBCs were performed on the Beckman Coulter DxH 800 hematology analyzer per standard protocol. CD34 cells were counted by flow cytometric ISHAGE protocols. Data from the DxH (48 variables per specimen) were exported into a data matrix with the corresponding flow cytometric data. Multiple regression analysis was performed using a step-wise method with log(peripheral CD34) as the dependent variable (SPSS, IBM). Data were randomly selected into a training-set of 70% of cases and a test-set of 30% of cases for validation. The derived model was further tested against peripheral blood data from the morning of collection to predict harvest yields. Further analyses were performed using Prism (GraphPad).
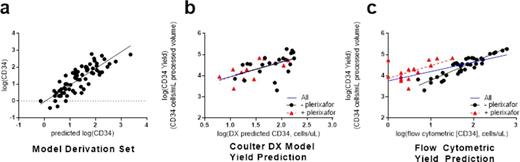
Results: Tandem peripheral blood CD34 counts and CBC cell-population data were obtained from 69 blood samples in 64 patients. The population included patients with multiple myeloma (45), non-Hodgkin lymphoma (12), Hodgkin lymphoma (5), and amyloidosis (2). 41% of patients were female. In the test data set examining collection yields, 37 patients were mobilized with GCSF (+/- chemotherapy) alone, while 17 had plerixafor added to the regimen. 33 of these patients had same-day CBC data available for model prediction. The median processed volume was 15 L (range 5.9 to 19.7). The model to predict peripheral CD34 counts incorporated 3 variables from the hematology analyzer data (SD-V-EGC, SD-C-EGC, and NE#). Interestingly, the model included two variables descriptive of the morphology of early granulocytic cells. The model demonstrated an R value of 0.829 (adjusted R2 = 0.670, figure 1a). In testing the morning-of-collection model-predicted peripheral CD34, we found the model performed similarly to flow cytometry in predicting 1st collection yields. Furthermore, the CD34 prediction using the model (Figure 1 b) resulted in similar correlation with first-collection yields in patients treated with plerixafor versus patients not treated with plerixafor, in contrast to day-prior CD34 counts by flow-cytometry (Figure 1c). Two outliers for CD34 cell yield based on model predicted peripheral CD34 were identified. In one patient, the processed volume was very low (6.8 L, <5% percentile), while the second had a low mononuclear cell collection efficiency (35%) compared to the mean in this population (58.7%±23.3%). Threshold values for the model accurately identified patients appropriate for collection initiation (or plerixafor administration).
Conclusion: Using data from a common, automated CBC analyzer, we developed a rapid, less-costly, and simple model to predict CD34 cell counts and 1st harvest yields. Because the measurement results can be obtained within the same clinic visit, and can be repeated with each CBC, the model is particularly useful to guide optimal use of plerixafor. We also envision that the model is useful for quality assurance of collection by identifying patients in whom cell yields were sub-optimal with respect to predicted CD34 cell counts. Additional studies to test the model in a larger population are ongoing. We propose that this model (and similarly derived models) can be implemented in clinical planning algorithms to improve the efficiency and cost of stem cell collection by apheresis.
Acknowledgments: We would like to acknowledge and the nurses and staff of the apheresis unit and the stem cell and flow cytometry laboratories at the Hospital of the University of Pennsylvania for their contributions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal