Abstract
Introduction: Graft-versus-host disease (GvHD) mediated by donor alloreactive T lymphocytes is the major obstacle of allogeneic hematopoietic stem cell transplantation (HSCT). Acute (aGvHD) and chronic GvHD (cGvHD) accounts for up to 40% and 50% of mortality, respectively following HSCT. Current therapy is based on suppression of the host's immune system, making the patient vulnerable to infections and tumor recurrence. T-cell depletion from the graft reduces the risk for GvHD but increases risks of delayed immune reconstitution leading to life-threatening infections.
Fas Ligand (FasL) has been shown to induce selective apoptosis of alloreactive T cells while sparing early hematopoietic progenitors and hence not jeopardizing hematopoietic engraftment. A negative selection process, aimed to eliminate mature T cells based on functional differential sensitivity of hematopoietic cells to FasL-induced apoptosis (rather than surface markers based selection), may significantly improve transplant outcome as it generates a potent graft containing early T and NK cells important for engraftment as well as post-transplantation immune recovery and prevention of relapse. Previous studies have been conducted mainly in a haploidentical mouse-to-mouse transplant model (Askenasy et al, 2013). The present study was conducted using a xenograft rodent GvHD model transplanted with a fresh mobilized hematopoietic graft, as one of the steps to garner experience in man prior to clinical trials.
Method: Apheresis-derived mobilized hematopoietic cells were collected from a healthy donor upon obtaining informed consent. GvHD was assessed following intravenous transplantation of 5x106 human (h) CD45+ cells into NOD-scid IL2Rgamma-null (NSG) mice that were irradiated with 2cGy. Cells were washed twice. The human hematopoietic graft (20ml) was manipulated within 24 hours after collection and used for all study groups. The cells of the treatment group (n=10) were subjected to 4-hour incubation in the presence of FasL. The control groups underwent the same procedure but without incubation (control 1, n=9) or with incubation for 4 hours without FasL (control 2, n=10). The mice were monitored for GvHD occurrence up to 40 days after transplantation (Cooke at el., 1996), and results expressed as mean ±1 SEM. Engraftment was evaluated using FACS analysis for hCD45+ chimerism.
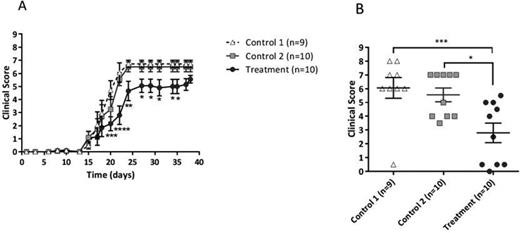
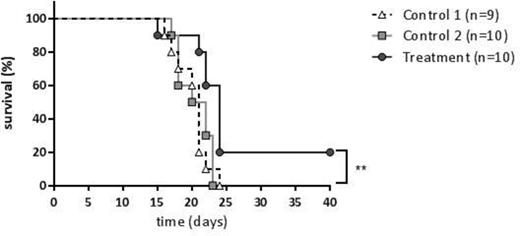
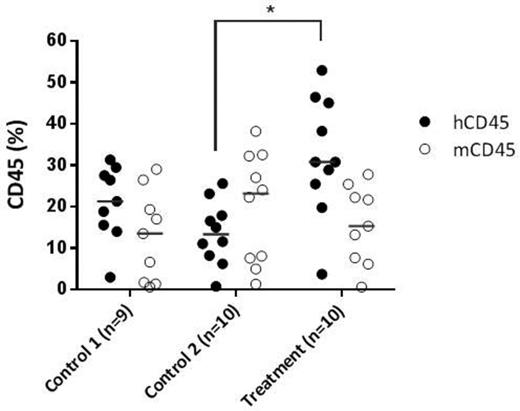
Results: Engraftment of hCD45+ cells was evident in all mice. The clinical score at day 40 post transplant was significantly lower in the treatment group in comparison to the control groups* (Fig 1 (A). On day 22 the average GvHD clinical score was 6.05±0.75, 5.5, and 2.84±0.708 for control 1, control 2 and treatment group, respectively (Fig 1B, p <0.05 and <0.001). In addition, Kaplan Meier analysis demonstrated extension of the survival curve following apoptotic treatment with FasL and 20% survival of the treated group. Median survival time (MST) was 21 days for both control groups and 24 days for the treatment group p<0.01 (Fig 2). Moreover, hCD45+ chimerism in the mice bone marrow was 1.5 fold and 2.36 fold higher in the treatment group compared to control 1 and 2, respectively (Fig 3). Conclusion: Taken together, these results demonstrate that apoptotic-based functional selection of the hematopoietic graft significantly reduced aGvHD without impairing human hematopoietic cell engraftment. Based on these data a phase I/IIa study is planned in subjects with hematologic malignancies undergoing matched related allo-HSCT to evaluate the safety and preliminary efficacy of GvHD prevention using apoptotic selected donor derived mobilized hematopoietic cells.
(*P<0.05,**P<0.01,***P<0.001, ****P<0.0001).
Meiron:Cellect Bio: Employment. Pinkas:Cellect Bio: Employment. Levi:Cellect Bio: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal