Abstract

Background: Myelodysplastic syndrome (MDS) therapeutic decisions have been traditionally based on the IPSS; however, this score system does not allow the identification of patients with low risk disease (low or intermediate-1 IPSS) but a poor prognosis, who could benefit from an early intervention. Garcia-Manero et al (Leukemia 2008) described a specific prognostic scoring system for this subgroup of patients (LR-PSS) based on age ≥60 years, hemoglobin <10g/dl, platelet count <50k/uL or 50-200k/uL, bone marrow blasts ≥4% and unfavorable cytogenetics (non-del(5q), non-diploid). This LR-PSS score system enables the stratification of low risk MDS patients into 3 different risk categories; interestingly, the third category identifies a subgroup of patients with a median overall survival (OS) similar to that of patients classified as intermediate-2 and high risk IPSS. Besides, the IPSS-R described by Greenberg et al (Blood 2012) has demonstrated a strong prognostic value for OS and LFS as compared to the IPSS when applied to different independent series of MDS patients. The prognostic impact of the LR-PSS has not been analyzed in MDS patients with very low-, low- and intermediate IPSS-R scores.
Aim: To analyze the prognostic impact according to OS and leukemia free survival of the LR-PSS when applied to a population MDS patients with very low, low and intermediate IPSS-R.
Methods: A total of 789 consecutive patients diagnosed with MDS (01/1992-12/2014) at the Catalan Institute of Oncology of Barcelona were included in the study. 413 (52%) had available cytogenetics and therefore, IPSS-R was calculated. Overall, 371 (89%) patients were classified as very low, low and intermediate IPSS-R and included in the study.
Results: 123 (30%) patients were classified as very low, 182 (44%) low and 66 (16%) intermediated IPSS-R risk MDS; median age 72 years (range 32-101) and 258 (69%) male. 1.4 % CRDU, 7.6 % RA, 41.6 % RCMD, 16.2 % RAEB‐1, 4.1 % RAEB‐2, 25.9 % CMML and 3.2 % MDS‐U with isolated 5q deletion according to the 2008 WHO classification. At diagnosis, median hemoglobin, platelet and bone marrow blast were 11.8 g/dL (5.5-17.1), 152 x109/L (1-1492) and 3 % (0-17), respectively and fifty-three (14.3 %) patients had unfavorable LR-PSS cytogenetics. For the whole population, median follow up was 6.6 years (range 6-7.7). At the time of last follow up, 48.2 % (179) had died and only 49 (13%) had progressed to acute myeloid leukemia.
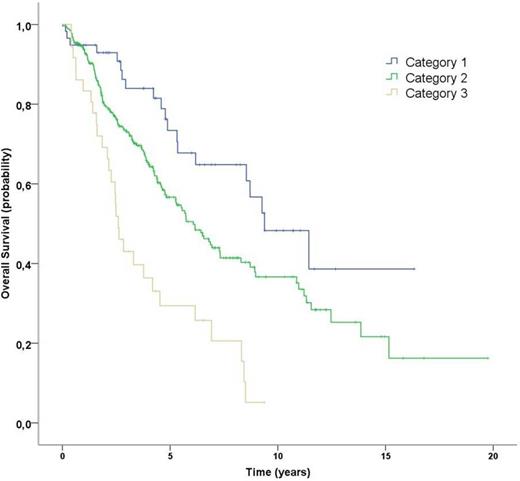
When the LR-PSS was applied to the very low, low and intermediate IPSS-R subgroups three well-differentiated prognostic categories could be identified: 58 patients (15.6%) category 1, scores 0-2; 277 (74.6%) patients category 2, scores 3-4 and 36 (9.8%) patients category 3, scores 5-7 with significantly different overall survival and leukemia free survival. Median OS for categories 1 (9.4 years; 95% CI 6.7-12), 2 (6 years; 95% CI 5-7.1) and 3 (2.6 years; 95% CI 2.1-3) were significantly different (p<0.001; Figure 1). Moreover, the rate of progression to acute myeloid leukemia was 5% (3/58), 13% (37/277) and 25% (9/36) for categories 1, 2 and 3, respectively.
Summary/Conclusion: When applied to a low risk (very low, low and intermediate) IPSS-R cohort of MDS population, the LR-PSS identifies a subgroup of patients with a significantly worse prognosis who could benefit from an early intervention. Further studies are warranted.
Kaplan-Meier survival for patients with very low-, low- and intermediate IPSS-R risk assigned to categories 1 to 3 by LR-PSS.
Kaplan-Meier survival for patients with very low-, low- and intermediate IPSS-R risk assigned to categories 1 to 3 by LR-PSS.
Sureda:Takeda: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal