Abstract
Reports in adults have shown that a BCR-ABL1 IS <10% at 3 months after the start of imatinib (IM) can predict better clinical outcome in chronic myeloid leukemia (CML). Recently, early molecular response (EMR) at 3 months has also been reported to correlate with better progression-free survival (PFS) in children treated with IM at a standard dose (260 mg/m2/day) (Millot et al, 2014).
In order to confirm the relevance of this cut-off in the pediatric population treated with high-dose IM, we investigated the impact a cohort of children and adolescents with CML in chronic phase (CP) followed at 11 Italian Centers.
Forty-four of 53 CP-CML patients treated with IM at a dose of 340 mg/m2/day who had available BCR-ABL1 levels at 3 months and had been followed for at least 12 months were included in this analysis. Cytogenetics were planned on bone marrow (BM) cells before and during IM therapy as well as molecular analysis on peripheral blood (PB) monthly and on BM every 3 months. Complete cytogenetic response (CCyR) was defined as the absence of Ph+ metaphases. Peripheral blood BCR-ABL1 levels were measured by quantitative RT-PCR assay expressed as International Scale (IS).
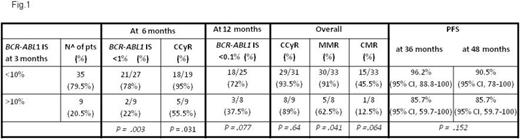
Major molecular response (MMR) was defined as ≤0.1% BCR-ABL1 IS, while molecular response (MR) was considered as ≤0.01% BCR-ABL1 IS. Complete molecular response (CMR) was used to indicate levels of disease ≤0.0032% BCR-ABL1 IS or undetectable. BCR-ABL1 transcript levels <10% 3 months after starting IM were considered as EMR and were used to assess the association between EMR and the rates of: a) BCR-ABL1 IS <1% and CCyR after 6 months of IM treatment; b) MMR at 12 months; c) CCyR at 6 months; d) overall CCyR, MMR and CMR, as well as the association between EMR and PFS.
Forty-four CP-CML patients - females: 17, males: 27; median age at diagnosis: 11.2 years (range: 3.1-15,8); median follow-up: 73.5 months (range:15-151.3) who had received IM at a median dose of 300 mg/m2/day (range: 140-380) were evaluable for molecular response. At 3 months of IM treatment, BCR-ABL1 transcript levels <10% and ≥10% were found in 79.5% and 20.5% of patients, respectively. The median administered dose of IM was similar (300 mg/m2 and 314 mg/m2 in patients with BCR-ABL1 IS <10% and ≥10%, respectively). At 6 months, 82% and 64% of evaluable patients showed CCyR and BCR-ABL1 transcript levels <1%, respectively. BCR-ABL1 transcript levels <0.1% were found in 63.5% of patients evaluable at 12 months. Overall, 92.5%, 85% and 39% of patients achieved CCyR, MMR and CMR, respectively. The correlations between BCR-ABL1 transcript levels <10% and ≥10% at 3 months and the rates of BCR-ABL1 IS <1% at 6 months and <0.1% at 12 months, CCyR at 6 months, overall CCyR, MMR and CMR are detailed in Fig 1. At 6 months, patients with BCR-ABL1 IS <10% after 3 months of IM had significantly higher response rates compared to those with BCR-ABL1 IS ≥10% (P = .031 and P.003 for CCyR and BCR-ABL1 IS <1%, respectively). Patients with EMR achieved higher rates of BCR-ABL1 IS <0.1% at 12 months as well as a better overall CCyR, MMR and CMR, though no statistically significant differences were found except for MMR (P =.041). With an overall PFS at 72 months of 91.4% (95% CI, 54.2-81.6), patients withBCR-ABL1 IS <10% at 3 months had a PFS similar to that of those with higher transcript levels. This might in part be explained by the high proportion (80%) of children who achieved a BCR-ABL1 IS <10% cut-off at 3 months. This response rate, higher than that (63%) reported by Millot in children treated with IM at a lower dose, is probably due to the higher dose of the drug utilized in our patients.
In conclusion, the high-doses of IM used in our study allowed to achieve better short and long term results in childhood CP-CML than those reported with lower doses of IM (Millot et al, 2014). Using such doses, the prognostic impact of a BCR-ABL1 IS <10% cut-off after 3 months of IM treatment as a surrogate marker of response at 1 year and PFS is not confirmed.
Saglio:BMS: Consultancy, Other: Fees for occasional speeches; Novartis: Consultancy, Other: Fees for occasional speeches; Pfizer: Consultancy, Other: Fees for occasional speeches ; ARIAD: Consultancy, Other: Fees for occasional speeches.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal