Abstract
Introduction: Imatinib mesylate (IM) is the first tyrosine kinase inhibitor (TKI) licensed for the treatment of chronic myeloid leukemia (CML). Severe bone marrow fibrosis (BMF) has been reported in excess of 40% of the patients with CML at diagnosis. Before TKIs became available, BMF which emerged at diagnosis and/or in the late periods of the disease was defined to be a poor prognostic factor, and it contributed significantly to morbidity and mortality from 10% to 30% in patients with CML. The relationship between BMF and both disease progression and prognosis has been the subject of re-evaluation after the introduction of IM therapy. In patients with CML, it has not been clearly demonstrated yet, whether IM improves the poor prognostic effect of fibrosis, and prevents the new BMF development or not.
Aim: The purpose of this study was to evaluate the effects of IM therapy on BMF formation, and the prognostic significance of BMF in patients with CML.
Material and Methods: One hundred and thirty-five CML patients were enrolled in the study. Patients' demographics, Sokal risk scores, molecular and cytogenetic responses and follow-up periods were noted from the patients' files retrospectively. All pre- and post-IM bone marrow biopsy samples, which were stained with hematoxylin and eosin, were re-evaluated for the current analysis. Grading of BMF was according to the European consensus decisions, graded as 0-III. The term "last bone marrow biopsy" (LBMB) is referred to a biopsy, which was performed at 18th months or later on during IM treatment.
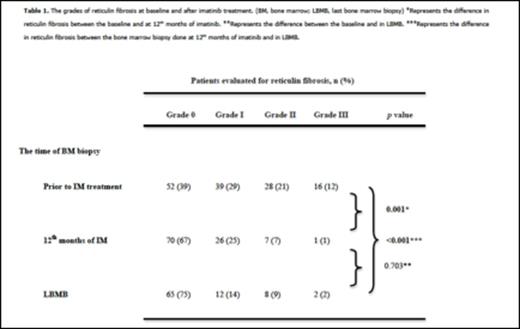
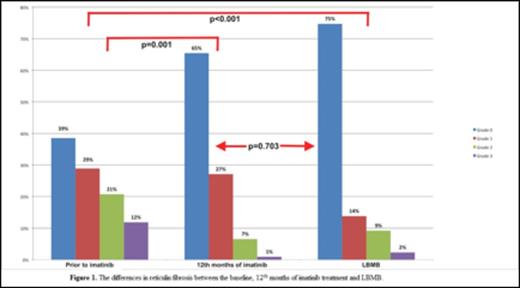
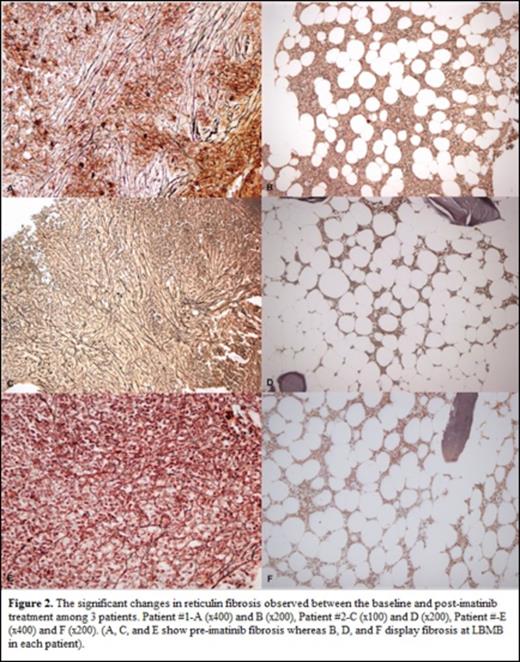
Results: The median age was 44 years (range, 18-92 years), and 78 patients (58%) were male. One hundred and twenty-eight patients (95%) were in chronic phase [CP], 4 patients (3%) were in accelerated phase [AP], and 3 patients (2%) were in blast crisis [BC] at the time of IM initiation. Out of 128 CML-CP patients, one hundred and twenty patients (93%) were in early CP, whereas 8 (7%) were in late CP. The percentage of low, intermediate, and high Sokal risk scores were 35%, 43%, and 22%, respectively. Before IM was initiated, thirty-one patients had received previous treatment modalities (hydroxyurea (HU) in twenty-one, and 10 patients had received interferon plus HU. he median duration of IM treatment was 45 months (range, 2-106 months). The rates of complete hematological response (CHR) at 3rd month, complete cytogenetic response (CCyR) at 12th month, and major molecular response (MMR) at 18th month were 92.4%, 71.6%, and 67.6%, respectively. BMF before the initiation of IM therapy was grade 0 in 52 patients (39%), grade I in 39 patients (29%), grade II in 28 patients (21%), and grade III in 16 patients (12%). There was a positive correlation between the Sokal risk scores and the grades of BMF at diagnosis (r:0.313, p <0.01), and as the Sokal risk scores increase, the grades of BMF also increase and the difference was significant (p =0.025). Also the spleen size significantly differ according to the grade of BMF, and the patients with a higher grade of BMF also had a larger spleen (p <0.001). The control bone marrow biopsies at the 12th month of IM were available in one hundred and four patients, and 70 (67%) of them have grade 0, 26 (25%) of them have grade I, 7 (7%) of them have grade II, and 1 (1%) of them has grade III BMF. After 12 months of IM treatment, the grades of BMF have significantly decreased when compared to the pre-treatment values (p =0.001), and BMF grades in LBMB has shown to be significantly decreased when compared to the pre-treatment values (p <0.001) (Table 1 and Figures 1&2). There was no significant difference regarding the grades of BMF, between the biopsy at 12th months and LBMB (p =0.703).
The CCyR rates at 12th month did not differ according to the pre-imatinib BMF grades (p =0.127). There was no significant difference between patients with or without CCyR at 12 months of IM regarding grades of BMF (p =0.785). The MMR rates at 18 months did not differ according to pre-treatment grades of BMF (p =0.112). There was no significantly difference in overall survival rates between initial BMF mild (grade 0-I) and severe (grade II-III) groups (p =0.278).
Conclusion: IM can reduce BMF after a long period of follow-up, independently from the molecular and cytogenetic responses. The BMF grades at diagnosis does not have a negative impact on the response to IM treatment. Therefore, the adverse prognostic impact of the marrow fibrosis among CML patients seems to disappear in the era of the TKIs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal