Abstract
Aberrant function of adipose tissue (AT) is seen in several diseases including cancer. Studies show that AT facilitates the progression of tumors through paracrine signaling of adipokines as well as regulation of cancer cell metabolism. However, the mechanism by which cancer cells corrupt the normal function of AT to gain proliferative and survival advantages is unknown. Using a murine model of blast crisis CML, we have shown enrichment of phenotypically primitive leukemia cells (Sca+/lin- leukemia cells, termed "PLCs") in the gonadal AT (GAT) as well as a fatty acid oxidation (FAO) regulatory role of AT. In this study, we evaluated the functional alteration of GAT in leukemic mice. We hypothesized that resident leukemia cells change the characteristics of GAT to obtain metabolic benefits.
To test this hypothesis, we first examined whether PLCs in GAT differed from PLCs in other tissues including bone marrow, spleen and peripheral blood. To this end, we utilized RNA-seq to obtain a genome-wide transcriptional profile of PLCs in different tissues. We found PLCs in GAT had a distinct gene expression pattern with enrichment of inflammatory response genes. Specifically, pro-inflammatory cytokines and chemokines were highly expressed by PLCs in GAT (Figure 1). Furthermore, the expression of those genes was also increased in the stromal vascular fraction (SVF) of GAT, indicating resident leukemia cells induced inflammation in GAT. Collectively, these results suggest that leukemia cells found in GAT are distinct from leukemia cells in other tissues and may alter the function of GAT.
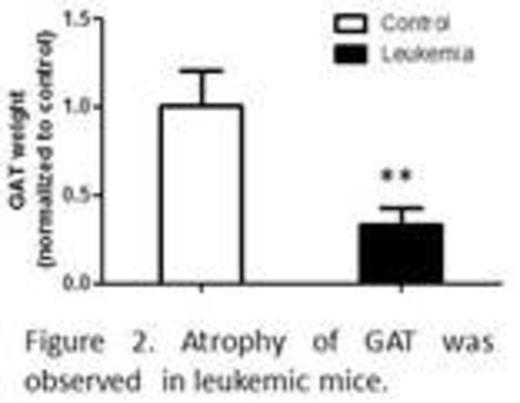
Another characteristic observed in our model was atrophy of GAT (Figure 2) as well as loss of body weight during leukemia progression, indicating the presence of cancer cachexia. Loss of GAT was also found prior to loss of body weight, suggesting the presence of a pre-cachexia stage. We speculated that atrophy of GAT was due to lipolysis induced by inflammation. Indeed, leukemic GAT released more free fatty acid (FFA) and had a lipolytic pattern of adipokines compared to normal GAT. Elevated FFA and lipolytic adipokines were also detected in leukemic serum. Together, these observations demonstrate that GAT in leukemic mice is lipolytic.
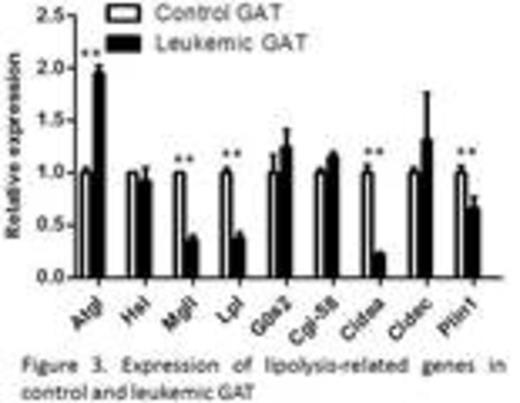
To gain insights into mechanisms involved in lipolysis of leukemic GAT, we examined expression of lipolysis-related genes (Figure 3). We found that leukemic GAT had increased expression of the adipose triglyceride lipase (Atgl), which is a rate-limiting lipase controlling lipolysis, and reduced expression of lipoprotein lipase (Lpl), whose expression correlates with the influx of fatty acids into adipocytes. Additionally, decreased expression of the cell death activator CIDE-A (Cidea), which is a lipid droplet (LD) associated protein that shields LDs from lipases and inhibits lipolysis, was found in leukemic GAT. Together, these findings suggest that regulation of lipid metabolism is disrupted in leukemic GAT, leading to lipolysis.
To test whether resident leukemia cells contribute to the atrophy of GAT, we examined the lipolytic effect of the pro-inflammatory cytokines and chemokines that were highly expressed by PLCs in GAT. We found that IL-1β and CSF2 induced lipolysis and engendered similar gene expression patterns of lipolysis-related genes in 3T3-L1 adipocytes. Notably, palmitate induced the expression of IL-1β in leukemia cells while it had an opposite effect in naive hematopoietic cells, implying a positive feedback loop where inflammation induces lipolysis which induces IL-1β which in turn augments inflammation. Additionally, an increased amount of IL-1β was observed in leukemic serum. Taken together, these data suggest that resident leukemia cells contribute to the atrophy of GAT through paracrine signaling of pro-inflammatory agents. This phenomenon appears to benefit leukemia cells by fostering FAO and metabolic properties that enhance leukemia cell survival.
Thus, targeting pathways that mediate inflammation and/or lipolysis may create a microenvironment that is less favorable to leukemia cells.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal