Abstract
Background: Although mantle cell lymphoma (MCL) has traditionally been considered an aggressive lymphoma with shortened survival, the long-term outcomes and initial presentation can be heterogeneous. Martin et al (JCO 2009) reported that 32% of patients with MCL at an academic referral center deferred therapy for at least 3 months, with a median overall survival (OS) of 64 months for patients treated within 90 days of diagnosis and median OS not reached for those who deferred therapy. We used the National Cancer Database (NCDB) to perform a national cohort analysis of the impact of deferred therapy in MCL.
Methods: The NCDB is a nationwide oncology outcomes database sponsored by the Commission on Cancer of the American College of Surgeons and the American Cancer Society, capturing nearly 70% of all newly diagnosed cases of cancer in the United States. We included all patients ≥18 years old who received initial treatment for newly diagnosed MCL in 2004-2011. MCL patients were identified by the International Classification of Diseases for Oncology code 9673 and variables of interest were captured using the Facility Oncology Registry Data Standards. Patients were determined to have received deferred therapy if their time to initial treatment was > 90 days. Chi-square tests were used as appropriate to compare baseline characteristics between immediate and deferred treatment groups, and OS was estimated using the Kaplan-Meier method. Log-binomial regression models were developed to identify characteristics associated with deferred treatment and multivariable Cox proportional hazard models were fit to evaluate the relationship between deferred treatment and OS.
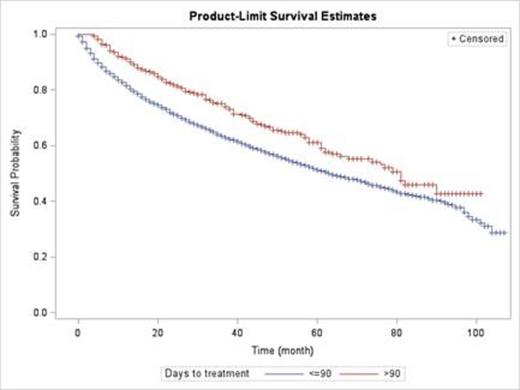
Results: Of 8209 patients with MCL, 492 (6.1%) received therapy > 90 days from diagnosis with a median time to treatment for this group of 121 days (range 91-1152). Among all patients, 64% were > 60 years of age, 73% were male, 85% were stage III/IV, and 83% had primarily nodal disease. Additional comorbidities were identified in 22% of patients, and 28% of patients presented with B-symptoms at diagnosis. Approximately 1/3 of patients received therapy in a high volume teaching/research institution. Compared to patients treated within 90 days of diagnosis, patients receiving deferred therapy were more likely to have early stage disease (22% vs 15% p<0.0001), extranodal presentation (24% vs 17%, p<0.0001), to be located in the Northeast region (26% vs 20%, p<0.0001), and to be treated at a high volume teaching/research institution (41% vs 33%, p=0.005). Patients treated within 90 days of diagnosis more commonly had B-symptoms (29% vs 16%, p<0.0001). There were no significant differences between the two groups with regard to gender, age, year of diagnosis, socioeconomic status (based on location of residence), or primary payer. When analyzed in a multivariable model, lack of B-symptoms (RR 1.67, 95% CI 1.38-2.03, p < 0.0001) and extra-nodal status (RR 1.24, 95% CI 1.00-1.53, p = 0.0468) were two strong clinical predictors of deferred therapy. Multivariable analysis demonstrated improved OS for patients who received deferred therapy (HR 0.79: 95% CI 0.67-0.93, p = 0.005; See Figure 1). Additional significant predictors of improved OS included age ≤ 60 years (HR 0.60: 95% CI 0.54-0.66, p < 0.0001), early stage disease (HR 0.66: 95% CI 0.59-0.74, p < 0.0001), lack of B-symptoms (HR 0.75: 95% CI 0.70-0.81, p < 0.0001), and lack of comorbidities (HR 0.63: 95% CI 0.58-0.68, p < 0.0001). Non-Hispanic black patients had inferior OS compared to the other racial/ethnic groups. Among patients who deferred therapy, male gender (p=0.046), age ≤ 60 years (p=0.0002) and lack of comorbidities (p<0.0001) were associated with improved OS, while remaining variables including region, stage, race, B-symptoms, and extranodal presentation were not.
Discussion: This national cohort analysis supports prior reports that deferred therapy in MCL is safe for a subgroup of patients with MCL. We found that deferred therapy > 90 days was associated with improved OS and that lack of B-symptoms was a strong predictor for deferred therapy. Predictors of improved survival for patients deferring therapy included young age and lack of comorbidities. These data support use of watchful waiting approach for well-selected newly diagnosed MCL patients.
Overall survival for newly diagnosed patients with mantle cell lymphoma based on time to initiation of therapy.
Overall survival for newly diagnosed patients with mantle cell lymphoma based on time to initiation of therapy.
Cohen:BMS: Research Funding; Seattle Genetics: Consultancy; Pharmacyclics: Consultancy; Millennium: Consultancy; Celgene: Consultancy; Janssen: Research Funding. Flowers:Infinity Pharmaceuticals: Research Funding; Acerta: Research Funding; Millennium/Takeda: Research Funding; AbbVie: Research Funding; Gilead Sciences: Research Funding; Acerta: Research Funding; Gilead Sciences: Research Funding; Onyx Pharmaceuticals: Research Funding; Janssen: Research Funding; OptumRx: Consultancy; Spectrum: Research Funding; Seattle Genetics: Consultancy; Infinity Pharmaceuticals: Research Funding; Genentech: Research Funding; Millennium/Takeda: Research Funding; Genentech: Research Funding; Janssen: Research Funding; Onyx Pharmaceuticals: Research Funding; Pharmacyclics: Research Funding; Spectrum: Research Funding; Pharmacyclics: Research Funding; AbbVie: Research Funding; Seattle Genetics: Consultancy; Celegene: Other: Unpaid consultant, Research Funding; OptumRx: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal