Abstract
Introduction
While core-binding factor acute myeloid leukaemia (CBF AML) as defined by t(8;21)(q22;q22) or inv(16)(p13q22)/t(16;16)(p13;q22) has a favourable prognosis, 30-40% of patients still relapse after chemotherapy. Risk factors predictive for relapse include increasing age and white cell count (WCC), poor performance status and adverse-risk cytogenetics. Rising minimal residual disease (MRD) by molecular monitoring and receptor tyrosine kinase (RTK) mutations also predict higher risk of relapse (Yin et. al., Blood 2012; Jourdan et. al., Blood 2013).
Aims
1. Identify prognostic markers for CBF AML
2. Determine significance of persistent molecular positivity in complete remission (CR) post-treatment
Methods
We undertook a retrospective audit from 2001-2012 at 4 tertiary-level hospitals. The inclusion criteria were adult patients >18 years with de novo CBF AML treated with at least intermediate dose cytarabine. Co-variates included in univariate analysis and then multivariate analysis if predictive of overall survival (OS) and relapse-free survival (RFS) included age, WCC, sex, cytogenetics, RTK mutations (KIT and FLT3) and MRD (RUNX1-RUNX1T1 or CBFB-MYH11 bone marrow (BM) qPCR post-induction (MRD1). Univariate analysis was also performed for BM MRD after each consolidation cycle 1-4 (MRD2-5 respectively).
Results
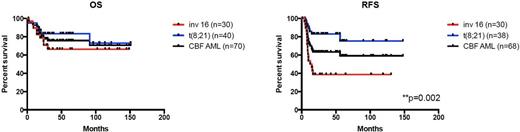
70 patients were identified (Male=39, Female=31; inv(16)=30, t(8:21)=40). The median age at diagnosis was 43 years (range 17-73). There were 2 induction deaths and 68 achieved morphological CR. OS was 70.7% and RFS was 59.1% at a median follow-up of 31.4 months. There were 16 deaths (inv(16)=9, t(8;21)=7; median OS 14.8 months; 9 from relapsed AML, 4 treatment-related complications, 2 graft-versus-host disease (GVHD) and 1 unrelated). 24 relapses (22 morphological, 2 molecular) occurred with a median RFS of 9 months (inv(16)=17, t(8;21)=7). RFS was significantly worse for inv(16) vs t(8;21) (39% vs 75%; p=0.0004). The inv(16) cohort had significantly higher median WCC of 33x109/L vs 10.5x109/L t(8;21). Univariate analysis identified age (p=0.032) and WCC>40 (p=0.002) as significant for inferior OS and RFS respectively. The impact of KIT (n=34, Pos=14, p=0.158) and FLT3 (n=27, Pos=2, p=0.152) mutations on OS/RFS were non-significant independent of CBF AML subtype. However, there were systematic differences in KIT and FLT3 data availability in the relapse vs non-relapse cohorts (Absent data: KIT 17/24(71%) vs 19/46(41%); FLT3 17/24(71%) vs 26/46(57%)). MRD analysis by qPCR at the different timepoints (MRD1=37, MRD2=24, MRD3=28, MRD4=23, MRD5=12) by < or ≥3 log reduction in comparison to pre-treatment values was not predictive of OS/RFS. On multivariate analysis excluding RTK mutations, age was the only significant predictor for OS (p=0.032) and WCC>40 for relapse (p=0.025). Standard vs intermediate/high-dose cytarabine in induction had no impact on OS/RFS but ≥3 consolidation cycles of intermediate-dose cytarabine improved OS vs ≤2 cycles (p=0.035). There was no significant difference in the median age of the cohorts receiving consolidation chemotherapy (≤2: n=37, 47 years, ≥3: n=30, 35.5 years).
Median BM qPCR values increased from 0 to 11% at relapse for inv(16) at a median duration of 4.3 months (range 1-8) and 0.05 to 178% for t(8;21) at 6 months (range 5-35) respectively. Of the 43 with durable CR, 28 maintained PB or BM qPCR values of 0-0.1% or <10 copy numbers throughout follow-up for 2 years post-completion of consolidation treatment. 6 had qPCR values >0.1% or >50 copy numbers; 5 were t(8;21) achieving PCR negativity at a range of 9-24 months post-completion of consolidation. Of the 24 who relapsed, 15 proceeded to stem cell transplant (13 allograft: inv(16)=8, t(8;21)=5; 2 autograft: inv(16)). There were 6 deaths in the allograft group (inv(16)=3, t(8;21)=3) and none in the autograft group. 3 deaths were related to relapsed disease post-allograft, 2 GVHD and 1 from non-GVHD complications.
Conclusions
Age is a significant predictor of OS in our CBF AML cohort while WCC is more predictive of relapse risk. The significance of RTK mutations and MRD is limited by data availability. ≥3 consolidation cycles of intermediate-dose cytarabine improved OS in comparison to fewer cycles. Stable low level MRD did not predict relapse. Regular monitoring of PB and BM qPCR values post-completion of treatment is necessary for prediction of subsequent relapse.
Grigg:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees. Szer:Alexion Pharmaceuticals Australasia Pty Ltd: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer Australia: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Shire Australia: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sanofi: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal