Abstract
Introduction: The management of patients with treatment resistant AML (failure to achieve complete remission, CR; or CR with incomplete blood count recovery; CRi) after intensive chemotherapy is an important clinical consideration. Anticipating the benefit of intensive salvage therapy facilitates patient management decisions and counseling. The UK Medical Research Council (MRC) has associated morphologic partial remission (PRm; defined as 5-15% bone marrow blasts) after course 1 of standard-dose cytarabine (SDAC) based induction, with 5yr overall survival (OS) outcomes comparable to achieving CR (42 vs 51%). In contrast, failure to achieve PRm was linked to 5-year OS of 20% (Wheatley, et al 1999). In an MD Anderson study, patients failing initial high-dose cytarabine (HiDAC) based induction had a 6-month OS expectation of only 7% (Ravandi, et al 2010). Less than 1% of patients in this study achieved PR using International Working Group (IWG) criteria (treatment related decrease in marrow blasts to 5-25% with a >50% reduction from baseline and blood count recovery. We therefore sought to verify the prognostic relevance of PRm in patients with treatment resistant AML (no CR/CRi).
Patients and treatment: A retrospective cohort of 104 patients failing intensive chemotherapy at 3 Australian hospitals (Alfred Hospital, Melbourne, Princess Alexandra and Royal Brisbane and Women's Hospitals, Brisbane) was identified. Prior therapy was standard-dose ara-C (SDAC) 100mg/m2 d1-7 in 73% or high-dose ara-C (HiDAC)(³1g/m2 cytarabine per dose for 5-8 doses) in 28% combined with idarubicin 9-12mg/m2 D1-3 as part of induction. For salvage after SDAC failure, the commonest regimens were HiDAC based, fludarabine and cytarabine (FLAG) variants or a second cycle of 7 + 3, the HiDAC group received further HiDAC based therapy, or FLAG based regimens. Outcomes were compared to a contemporaneously treated AML population (n=128) achieving CR/CRi.
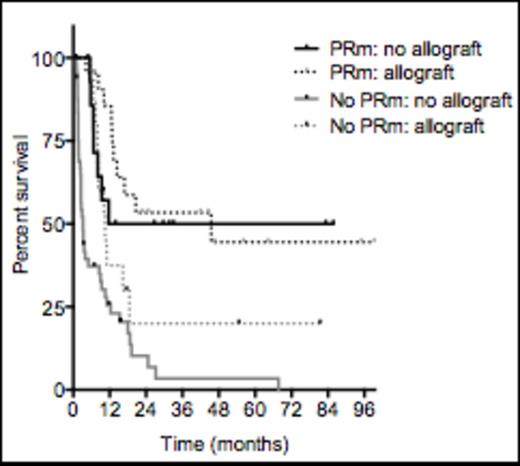
Results: OS was stratified according to the level of residual bone marrow blasts after induction. Patients with 5-15% residual blasts (PRm) had a median OS of 20.6 mo, compared to only 5.0 mo for patients with a residual blast count >15% (p<0.0001). Outcome was superior in patients achieving a marrow blast reduction of ³50% or greater after induction (median OS 18.7m, vs 5.5m if blast reduction was <50%; p >0.0001). The proportion of patients with treatment resistant AML (no CR/CRi) achieving PRm was 41%. CR/CRi rates from salvage chemotherapy were 64% for those failing SDAC and 52% for those failing prior HiDAC-based induction (p=0.37). The likelihood of attaining subsequent remission SDAC-based induction failure was not related to PRm status after cycle 1 of therapy (CR/CRi 73%, compared to 66% without prior mPR; p=0.85). In contrast, the response to subsequent salvage chemotherapy was more common after attainment of prior PRm in cycle 1 for those receiving HiDAC-based induction (CR/CRi 83%, compared to 14% without prior PRm; p=0.01). For patients receiving prior SDAC-based induction, median OS was not reached for patients with PRm, compared to only 8 mo for those not achieving PRm (p=0.0006) (Fig 1A). For patients receiving prior HiDAC-based induction, median OS was 45.5 mo for patients with PRm, compared to only 3.3 mo for those not achieving PRm (p<0.0001) (Fig 1). If PRm was achieved after cycle 1 of induction, outcomes were not improved by subsequent HSCT (median OS 45.5 mo with HSCT, compared to 48.8 mo without HSCT [p=0.2]) (Fig 1B). In contrast, the benefit of HSCT was greater for resistant patients failing to achieve PRm (median OS 10.5 mo with HSCT, compared to 3.2 mo without [p=0.006]) (Fig 1B).
Conclusion: in patients with AML failing initial chemotherapy, good long-term outcomes are still achievable, especially if a PRm was achieved after the first course of induction chemotherapy, regardless of whether SDAC or HiDAC induction was delivered. In contrast, patients refractory (no CR or PRm) to induction chemotherapy have a very poor prognosis and should be considered candidates for experimental therapies or allogeneic stem cell transplantation. Assessment for PRm may be a useful prognostic factor when clinical decisions regarding adults with AML failing to achieve CR/CRi after induction therapy are being considered.
Ð Survival by response, by induction intensity
Ð Survival after induction failure and by prior PRm status and subsequent allograft
Ð Survival after induction failure and by prior PRm status and subsequent allograft
Mollee:Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Onyx: Membership on an entity's Board of Directors or advisory committees. Wei:Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees; Servier: Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Membership on an entity's Board of Directors or advisory committees, Research Funding; Agios: Membership on an entity's Board of Directors or advisory committees; Astra Zeneca: Membership on an entity's Board of Directors or advisory committees; Bayer: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal