Abstract
Background: Improvements in the early identification of older patients with a high post-operative VTE risk would potentially translate into more effective VTE prevention and management strategies.
Objectives: We sought to establish whether measuring early indices of in vivo platelet activation following orthopedic surgery predicted VTE in older patients.
Methods: We performed a prospective cohort study in 32 patients undergoing elective hip or knee arthroplasty who received warfarin thromboprophylaxis post-operatively. Patients were assessed for deep vein thrombosis post-operatively by compression ultrasonography (CUS) and followed for 30 days for clinical thrombotic events. Circulating levels of platelet-monocyte aggregates (PMAs), platelet surface p-selectin expression, and integrin αIIbβ3 activation were assessed immediately pre-operatively and on post-operative day 1 by flow cytometry. The procoagulant markers d-dimer and fibrinogen were measured in parallel.
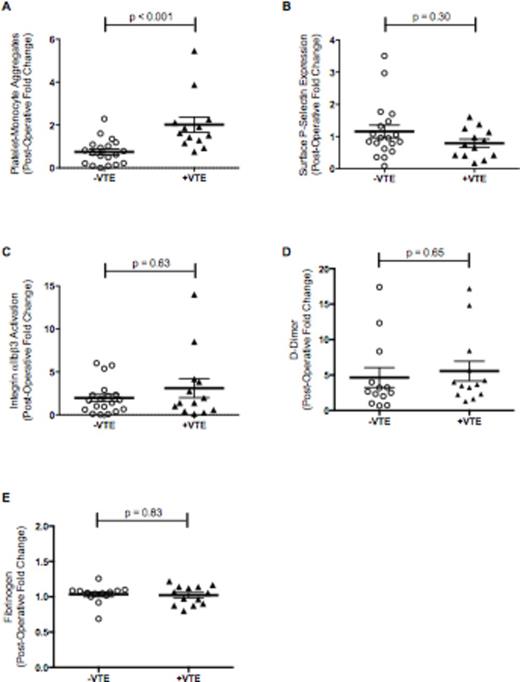
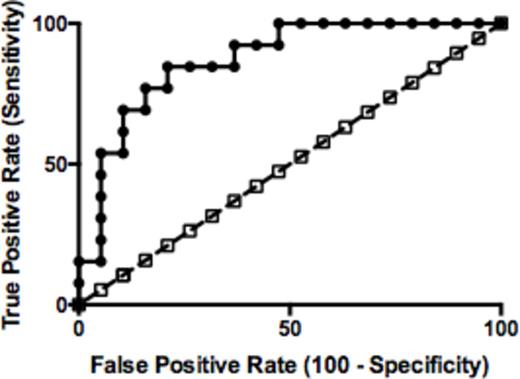
Results: The average age was 65.6±7.1 years and 43.8% were male (Table 1). VTE occurred in 40.6% (n=13/32) of patients a median of 3 days (IQR 2-3) after surgery. The majority of thrombotic events were deep vein thromboses that altered clinical management. Baseline clinical characteristics, age, weight, and laboratory values did not differ between patients who developed VTE post-operatively and those that did not. Post-operatively, circulating levels of PMAs were significantly increased in patients with VTE but essentially unchanged in patients without VTE (post-operative fold-change 2.02±0.36 vs. 0.75±0.14, p<0.001; Figure 1). P-selectin expression and integrin αIIbβ3 activation were not associated with VTE. Similarly, neither d-dimer nor fibrinogen predicted VTE. Receiver operating curve characteristic analyses demonstrated that increased circulating PMA levels performed well for predicting patients who developed VTE (AUC 0.87, 95% CI 0.75-0.99; p < 0.001) with a sensitivity and specificity of 77% and 83%, respectively (Figure 2).
Conclusions: Increased circulating PMAs measured on post-operative day 1 are an early marker predicting VTE following orthopedic surgery in older adults.
Characteristics of the patients with and without venous thromboembolism (VTE; central tendency data are reported as mean (±SD) unless otherwise specified; BMI: body mass index; DJD: degenerative joint disease; aPTT: activated partial thromboplastin time; *p < 0.05 versus without VTE).
| . | Overall (n=32) . | Without VTE (n=19) . | With VTE (n=13) . | P value . |
|---|---|---|---|---|
| Age, years | 65.6 ± 7.1 | 65.6 ± 8.0 | 65.5 ± 5.7 | 0.95 |
| Male Gender, n (%) | 14 (43.8%) | 7 (36.8%) | 7 (53.8%) | 0.91 |
| BMI, kg/m2 | 30.8 ± 6.5 | 30.4 ± 6.5 | 31.4 ± 6.7 | 0.67 |
| Obesity (BMI ³ 30kg/m2), n (%) | 17 (53.1%) | 8 (47.4%) | 8 (61.5%) | 0.43 |
| Baseline, Pre-operative Values | ||||
| Hemoglobin, mg/dL | 13.6 ± 1.2 | 13.5 ± 1.3 | 13.9 ± 1.1 | 0.29 |
| Platelets, K/uL | 282 ± 62 | 274 ± 52 | 292 ± 75 | 0.44 |
| White Blood Cell Count, K/uL | 7.4 ± 2.6 | 7.4 ± 3.1 | 7.3 ± 1.8 | 0.99 |
| INR | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.91 |
| Prothrombin Time, sec | 13.1 ± 0.6 | 13.1 ± 0.7 | 13.1 ± 0.7 | 0.92 |
| aPTT, sec | 31.4 ± 3.7 | 31.0 ± 2.4 | 32.0 ± 5.1 | 0.45 |
| Fibrinogen, mg/dL | 374 ± 70 | 391 ± 61 | 351 ± 77 | 0.13 |
| D-Dimer, µg/mL | 0.8 ± 0.8 | 0.8 ± 1.0 | 0.8 ± 0.6 | 0.94 |
| C-reactive protein | 6.8 ± 14.3 | 9.5 ± 18.6 | 3.3 ± 2.8 | 0.25 |
| Type of Surgery | ||||
| Total knee arthroplasty (TKA), n (%) | 23 (71.9%) | 13 (68.4%) | 10 (76.9%) | 0.70 |
| Unilateral TKA, n (%) | 20 (62.5%) | 13 (68.4%) | 7 (53.8%) | 0.07 |
| Bilateral TKA, n (%) | 3 (9.4%) | 0 (0%) | 3 (100%) | 0.07 |
| Total hip arthroplasty (THA), n (%) | 9 (29.1%) | 6 (31.6%) | 3 (23.1%) | 0.70 |
| Tourniquet time (for TKA), min. | 56.1 ± 12.6 | 55.5 ± 16.0 | 56.9 ± 7.0 | 0.80 |
| . | Overall (n=32) . | Without VTE (n=19) . | With VTE (n=13) . | P value . |
|---|---|---|---|---|
| Age, years | 65.6 ± 7.1 | 65.6 ± 8.0 | 65.5 ± 5.7 | 0.95 |
| Male Gender, n (%) | 14 (43.8%) | 7 (36.8%) | 7 (53.8%) | 0.91 |
| BMI, kg/m2 | 30.8 ± 6.5 | 30.4 ± 6.5 | 31.4 ± 6.7 | 0.67 |
| Obesity (BMI ³ 30kg/m2), n (%) | 17 (53.1%) | 8 (47.4%) | 8 (61.5%) | 0.43 |
| Baseline, Pre-operative Values | ||||
| Hemoglobin, mg/dL | 13.6 ± 1.2 | 13.5 ± 1.3 | 13.9 ± 1.1 | 0.29 |
| Platelets, K/uL | 282 ± 62 | 274 ± 52 | 292 ± 75 | 0.44 |
| White Blood Cell Count, K/uL | 7.4 ± 2.6 | 7.4 ± 3.1 | 7.3 ± 1.8 | 0.99 |
| INR | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.91 |
| Prothrombin Time, sec | 13.1 ± 0.6 | 13.1 ± 0.7 | 13.1 ± 0.7 | 0.92 |
| aPTT, sec | 31.4 ± 3.7 | 31.0 ± 2.4 | 32.0 ± 5.1 | 0.45 |
| Fibrinogen, mg/dL | 374 ± 70 | 391 ± 61 | 351 ± 77 | 0.13 |
| D-Dimer, µg/mL | 0.8 ± 0.8 | 0.8 ± 1.0 | 0.8 ± 0.6 | 0.94 |
| C-reactive protein | 6.8 ± 14.3 | 9.5 ± 18.6 | 3.3 ± 2.8 | 0.25 |
| Type of Surgery | ||||
| Total knee arthroplasty (TKA), n (%) | 23 (71.9%) | 13 (68.4%) | 10 (76.9%) | 0.70 |
| Unilateral TKA, n (%) | 20 (62.5%) | 13 (68.4%) | 7 (53.8%) | 0.07 |
| Bilateral TKA, n (%) | 3 (9.4%) | 0 (0%) | 3 (100%) | 0.07 |
| Total hip arthroplasty (THA), n (%) | 9 (29.1%) | 6 (31.6%) | 3 (23.1%) | 0.70 |
| Tourniquet time (for TKA), min. | 56.1 ± 12.6 | 55.5 ± 16.0 | 56.9 ± 7.0 | 0.80 |
Circulating numbers of platelet-monocyte aggregates (Panel A) were increased post-operatively in patients with VTE (+ VTE, n=13), compared to patients without VTE (- VTE, n=19). In comparison, neither platelet surface p-selectin expression (Panel B) nor integrin αIIbβ3 activation (Panel C) predicted the development of VTE. Similarly, neither d-dimer (Panel D) nor fibrinogen (Panel E) predicted VTE (bars show mean±SEM).
Circulating numbers of platelet-monocyte aggregates (Panel A) were increased post-operatively in patients with VTE (+ VTE, n=13), compared to patients without VTE (- VTE, n=19). In comparison, neither platelet surface p-selectin expression (Panel B) nor integrin αIIbβ3 activation (Panel C) predicted the development of VTE. Similarly, neither d-dimer (Panel D) nor fibrinogen (Panel E) predicted VTE (bars show mean±SEM).
ROC analyses demonstrated that post-operative changes in circulating PMA levels performed well for identifying patients who developed VTE (area under the ROC curve of 0.87, 95% CI 0.75-0.99; p < 0.001).
ROC analyses demonstrated that post-operative changes in circulating PMA levels performed well for identifying patients who developed VTE (area under the ROC curve of 0.87, 95% CI 0.75-0.99; p < 0.001).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal