Abstract
Background
Acute chest syndrome (ACS) is the second most frequent reason for hospitalization in children and adults with sickle cell disease (SCD) and the most common cause of death. Physicians caring for SCD patients need to be aware of the early symptoms and signs of ACS, assessment of ACS severity to guide optimal therapy, and measures to prevent ACS. Recently there is some consensus on the definition of ACS, and an ACS severity assessment tool used in multicenter clinical research (Ballas et al. for the Investigators of the Comprehensive Sickle Cell Centers. Am J Hematol 2010) has been utilized but not validated in a real-world setting. Thus, existing guidelines and policy statements for the management of children with ACS do not provide a uniform system for grading of severity and management, and the new guidelines from NHLBI for sickle cell disease management by primary care physicians does not rectify this situation [2014 NIH guidelines].
In contrast, the evidence base for role of incentive spirometry in preventing ACS (Bellet et al, NEJM 1995)and decreasing severity of ACS is strong/moderate and accordingly incentive spirometry recommendations are included in guidelines [2014 NIH guidelines, Crabtree et al. Pediatrics 2011]. As a first step toward this quality improvement initiative at our institution our objective was to assess the current knowledge of resident physicians and nursing regarding these 2 aspects of ACS: Severity assessment and Incentive spirometry.
Methods
This tertiary care teaching hospital admits over 20 sickle cell patients per month on the pediatric ward. Pediatric house staff learns about ACS management and prevention as part of 2 formal didactic sessions on SCD per year and bedside teaching by rotating pediatric hematology-oncology faculty, fellows, and advanced-practice nurses. Pediatric ward nurses have 1 didactic session on SCD per year. An anonymous survey consisting of ten items regarding the use of a scoring system for ACS and incentive spirometry was administered to 40 pediatric resident physicians and 20 pediatric inpatient nurses who routinely engage in care of pediatric patients hospitalized with ACS. Descriptive statistics were employed for analysis. This was followed by an education session on ACS for the group. This study was approved by the institutional IRB.
Results
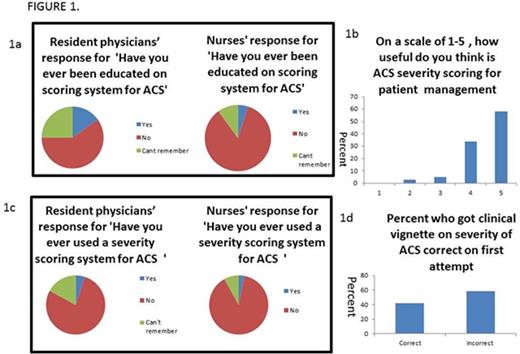
SEVERITY SCORING: We found that 15% of resident physicians and 5% of nurses had been educated on the use of a ACS severity assessment score in past (Fig 1a), however an overwhelming 92% felt that such a scoring system would be extremely useful for assessing their patient's condition and their management (Fig 1b). Only 5% of residents and 3% of nurses had used a severity scoring system for ACS in the past to guide their management decisions (Fig 1c). This was further confirmed by testing them on a clinical vignette based on ACS and a majority of the residents and nurses (58%) answered it incorrectly (Fig 1d).
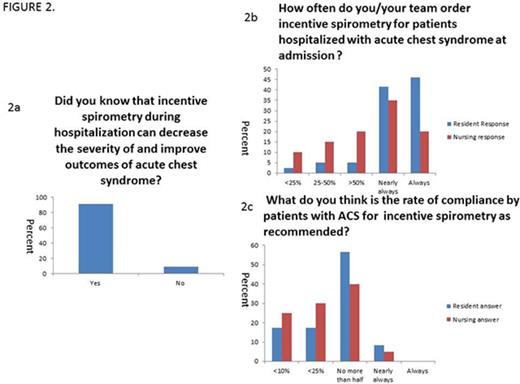
INCENTIVE SPIROMETRY: An impressive 91% responded they were aware that incentive spirometry during hospitalization can decrease the severity of and improve outcomes of acute chest syndrome (Fig 2a). Greater than 88% of resident physicians thought that incentive spirometry is almost always ordered for the patients but the same proportion felt that the patients are compliant less than 50% of the time with instructions regarding use (Fig 2b and 2c). Nurses' responses were more variable on the ordering of incentive spirometry for the patients but 95% thought that less than patients were compliant less than half the time with the orders (Fig 2b and 2c).
Conclusions
We conclude that the knowledge of resident physicians and nurses regarding severity assessment of acute chest syndrome is extremely limited and greater efforts are needed to educate and encourage them to include this assessment in their management decisions to improve their understanding of patient condition and optimize care. In addition, we found that importance of incentive spirometry is recognized by house staff, however, the patient compliance is far below desirable and stricter reinforcement will be needed by the physicians and nurses to potentially improve outcomes for hospitalized patients with ACS. This pilot study thus identifies room for quality improvement at several different steps in the process of care for SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal