Abstract
Disease Risk Index is the Major Predictor of Outcome Following Myeloablative Haploidentical Hematopoietic Stem Cell Transplantation (haplo-HSCT) and Post-Transplant Cyclophosphamide (PT/Cy)
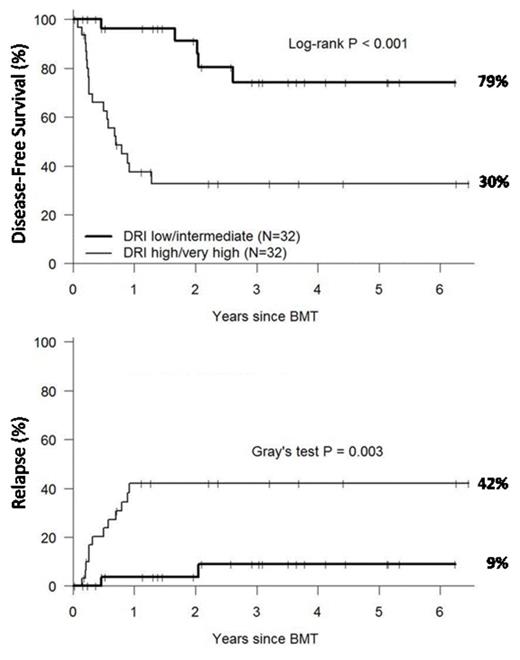
Although non-myeloablative (NMA) haplo-HSCT utilizing PT/Cy results in low rates of GVHD, infection, and non-relapse mortality (NRM), relapse remains the predominant cause of treatment failure, occurring in up to 50% of patients. To reduce the risk of relapse often associated with the use of NMA preparative regimens, we have developed a myeloablative haplo-HSCT utilizing PT/Cy. Sixty-four patients have been transplanted following either Busulfan-based (n=20) or TBI-based (n=44) myeloablative conditioning, T-cell replete PBSC infusion, PT/Cy, and tacrolimus/mycophenolate mofetil. Median age was 43 (range 21-60). Patient characteristics included a high/very high disease risk by the Dana-Farber/CIBMTR disease risk index (DRI) in 32 patients (50%), KPS<90 in 69%, and comorbidity index (CMI) of ≥2 in 58% of patients. The most common indications for transplant were AML, ALL, and advanced-phase CML in 55%, 20% and 12% of patients respectively. Median follow-up for surviving patients was 24 months. All patients have engrafted with no late graft failure. Grade II-IV, III-IV acute GVHD and moderate-severe chronic GVHD occurred in 46%, 23%, and 30% respectively. One-year NRM was 10%. Predicted three-year overall survival (OS), disease-free survival (DFS), and relapse are 53%, 53%, and 26% respectively. In multivariate analysis, high/very high DRI was the most significant negative predictor of OS (HR 13.26, p<0.001), followed by CMI≥2 (HR 3.54, p=0.01) and age (HR 1.26, p=0.038, per each 5 year increase in age). DRI was also significantly associated with DFS (HR 10.84, p<0.001), NRM (HR 15.0, p=0.004), and relapse (HR 8.85, p=0.004). In the 32 patients with standard risk disease (low/intermediate DRI), outcomes were significantly improved with one-year NRM of 0% and predicted 3-year OS, DFS, and relapse of 79%, 74% and 9% respectively. Conditioning regimen (TBI vs. Busulfan) had no significant impact on outcome. This analysis confirms that DRI is a strong predictor of outcome following myeloablative haplo-HSCT and PT/Cy and adds to a growing body of literature suggesting that haplo-HSCT is a safe and effective transplant option for patients lacking a matched sibling donor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal