Abstract

INTRODUCTION: Despite recent advances in treatment for MDS, allogeneic hematopoietic stem cell transplantation (alloHCT) remains the only curative therapy. Historically, patients (pts) 65 and older with Medicare did not have coverage for HCT. On August 4th 2010, the Centers for Medicare and Medicaid services (CMS) established coverage for HCT for MDS through coverage with evidence development (CED). A Center for International Bone Marrow Transplant Research (CIBMTR) study comparing outcomes of pts 55-64 vs. 65 and older was approved. Herein we report the survival outcomes of the first 688 pts enrolled on the study.
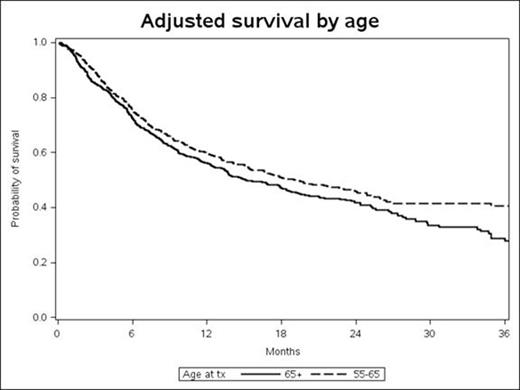
RESULTS: From 12/15/2010 to 5/14/2014, 688 pts 65 years and older (65+) underwent alloHCT for MDS compared with 592 pts 55-64 years (55-64). Median follow-up was 12 and 18 months for the 65+ and 55-64 group respectively. Median age was 68 and 61 for the 65+ and 55-64 group respectively. In the 65+ group, 76%, 22% and 2% were ages 65-69, 70-74 and > 74 years old. At the time of diagnosis, 30%, 10%, 42% were diagnosed with RA/RARS/RCMD/RCMDRS/5q-, CMML and RAEB respectively. The IPSS score at diagnosis was Low risk/intermediate-1 and intermediate-2/high risk in 39% and 31% respectively, and 23% had t-MDS. In the 55-64 group, 43% and 57% were 55-59 and 60-64 years old respectively. Otherwise, patient and disease characteristics were similar in both groups. More patients in the 55-64 group compared to 65+ group received a myeloablative alloHCT (49% vs. 29%). The donor was an HLA identical sibling in 24% vs. 34% in the 65+ vs. the 55-64 groups. Because of confounding between age and selection of transplant procedures (including preparative regimen intensity, graft source, gvhd prophylaxis) we chose to adjust only for patient and disease characteristics in the multivariate analysis (MVA). Age group 65+ vs. 55-64 had no significant impact on 100-day mortality (HR 1.26; CI 0.91-1.75 p=0.16) or overall survival (HR 1.14; CI 0.98-1.33 p=0.1) in the MVA. The adjusted 100 day survival was 84% vs. 87%, one year survival was 60% vs. 56% and 2 year survival was 42% vs. 46% in the 65+ group vs. 55-64 group respectively. As expected, MVA for 100 day mortality identified that poor cytogenetics (HR 1.85; CI 1.28-2.68) compared to good cytogenetics, patients with stable disease/no response to therapy (HR 3.35; CI 1.59-7.07), disease progression/relapsed disease (HR 2.91; CI 1.13-7.51), patients who did not receive any therapy prior to preparative regimen (HR 2.9; CI 1.17-7.21) compared to patients in complete remission and platelet count <50x109/L (H1.68; CI 1.17-2.43) compared to platelet ≥ 50 x 109/L at diagnosis were independently associated with worse outcome. MVA for overall survival identified that, 11-20% blasts in bone marrow at time of preparative regimen (HR 1.58; CI 1.24-2.03) compared to < 5% blasts, poor cytogenetics (HR 1.68; CI 1.4-2.01) compared to good cytogenetics and Sorror comorbidity index ≥ 4 (HR 1.59; CI 1.27-1.99) compared to Sorror comorbidity index 0 were independently associated with worse outcome.
CONCLUSION: In patients who are eligible for alloHCT, there was no difference in 100 day mortality or overall survival for patients 55-64 compared to patients 65 years and older. Age alone should not be a determinant for alloHCT eligibility.
Deeg:Medac: Research Funding; Medac: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal