Abstract
Background: Aplastic anemia (AA), paroxysmal nocturnal hemoglobinuria (PNH) and myelodysplastic syndrome (MDS) are the heterogeneous group of bone marrow failure syndrome (BMFs). AS they often show profound hypocellular marrow, the diagnosis is often difficult by bone marrow and laboratory examination alone. Red to yellow marrow conversion occurs with age in the appendicular skeleton (AS), where red marrow is converted to yellow marrow until the age of early 20s. Although abnormal distribution of red marrow in appendicular skeleton were previously reported in small series of patients with MDS, leukemia and lymphoma by MRI, no further study has published so far. Here, we examined distribution of red marrow in AS by low-dose multi-detector CT (MDCT) in BMFs patients, and analyzed the relationship between the abnormal medullary pattern in AS and laboratory variables. The relationship between the MDCT pattern and subsequent development of leukemic transformation on survivals was analyzed in patients with BMFs.
Patients: We retrospectively reviewed the medical records of 138 untreated patients (AA n=36, PNH n=5, and MDS n=97) with BMFs diagnosed in the Department of Hematology/Oncology at Kameda Medical Center, Kamogawa, Japan, from July 2008 to June 2014. Follow-up MDCTs were evaluated in 28 MDS patients when they were diagnosed as overt AML (MDS/tAML). Retrospective review of clinical and laboratory features including complete blood count, % of bone marrow blast, chromosomal analysis, and International Prognostic Scoring System (IPSS) at diagnosis was performed. WHO classification of patients with MDS was as follows: RCUD (n=21), RARS (n=2), RCMD (n=26), RAEB (n=43), and, MDS unclassified (MDS-U) (n=5). Leukemia-free survival (LFS) and overall survival (OS) were analyzed in 73 patients with MDS who were ≥65 years of age and ineligible for allogeneic stem cell transplantation (allo SCT) by the Kaplan-Meier.
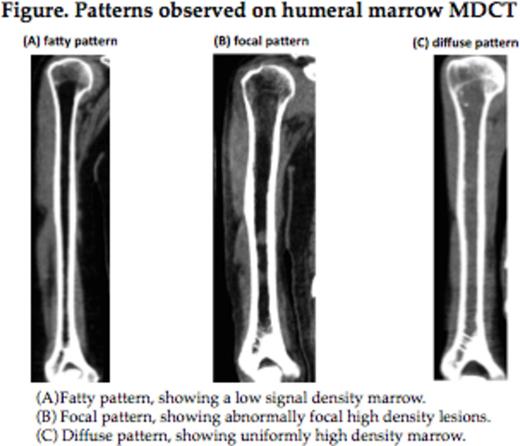
CT image acquisition and Image analysis: Non-enhanced CT examinations were performed from the skull to the knees by MDCT scanner (Aquilion 64, Tohshiba, Tokyo, Japan). Bony canal of humeral and femoral bone were visualized by coronal and sagittal axis image reconstruction. Medullary CT density of humerus and femurs were measured and the results were expressed as Hounsfield unit (HU). As the normal adult bone marrow was composed of rich adipocytes and called yellow marrow, it is represented by low density CT value between -30 to -100 HU. The value above -30 HU observed in long bony canals was considered as high density. Medullary pattern of AS were categorized as follows: (1) fatty pattern; showing a low signal density marrow (2) focal pattern; showing abnormally focal high density lesions (3) diffuse pattern; showing uniformly high density marrow.
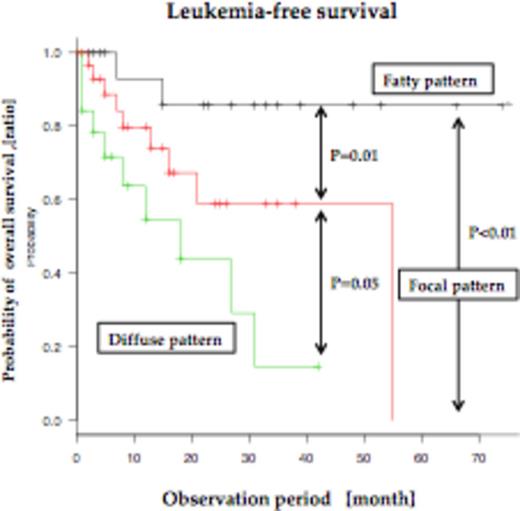
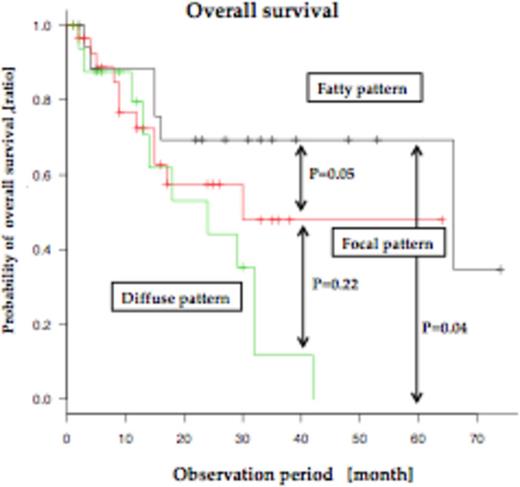
Results: All 36 patients with AA showed a fatty (n=13, 36.1%) or focal (n=23, 63.9%) pattern in medullary AS on MDCT, and none of them showed diffuse pattern. Five patients with PNH showed as follows: fatty/focal/diffuse, 1/3/1. Ninety-seven patients with MDS showed as follows: fatty/focal/diffuse, 24/46/27. Patients with MDS who showed diffuse pattern had a significantly low hemoglobin concentration compared to those with fatty or focal pattern (p=0.03). Among the patients with MDS, most of the patients with RCUD (n=21), RARS (n=2), RCMD (n=26), MDS-U (n=5) showed the fatty or focal pattern (fatty or focal/diffuse pattern; RCUD (18/3), RARS (2/0), RCMD (21/5), MDS-U (5/0)), but approximately half (46%) of patients with RAEB showed diffuse pattern (fatty/focal/diffuse pattern; 7/17/19). In addition, patients with transformed to MDS/tAML showed either focal (n=10, 35.7%) or diffuse (n=18, 64.3%) pattern and none of them showed fatty pattern. In 73 patients with MDS who were ≥65 years of age and ineligible for allo SCT, the group with focal or diffuse pattern had significantly shorter LFS and OS compared to the group with fatty pattern (p=0.01, p=0.05, respectively). Patients with focal pattern in AS showed longer LFS than those with diffuse pattern (p=0.05), but difference was not statistically significant in OS (p=0.22).
Conclusions: This study showed that MDCT imaging of the appendicular skeletons provided important information for the diagnosis and prognosis of patients with BM. In patients with MDS, focal or diffuse pattern on MDCT showed negative prognostic impact on LFS and OS, and these patterns appeared to reflect the status of disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal