Abstract

Background: An emerging goal of tyrosine kinase inhibitor (TKI) therapy for patients with CML is to achieve sustained deep molecular response. Several factors, such as efficacy and tolerability of therapy and patient or disease characteristics, may impact treatment success. In this study, the correlation between specified prognostic factors and predicted molecular response levels after 1 year of treatment with nilotinib (NIL) 300 mg twice daily or imatinib (IM) 400 mg once daily was evaluated.
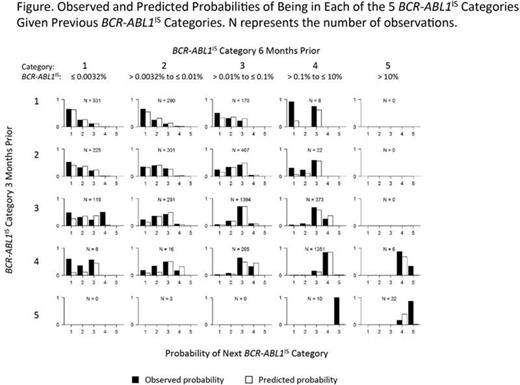
Methods: Datafrom the ENESTnd trial comparing frontline treatment with NIL vs IM, in which BCR-ABL1 transcript levels were assessed every 3 months by real-time quantitative polymerase chain reaction on the International Scale (IS), were used to develop a statistical regression model to predict the BCR-ABL1IS category of a patient at any time point after 1 year of therapy. Potential predictors investigated were treatment, EMR status (BCR-ABL1IS ≤ 10% at 3 months), gender, age, Sokal risk score, BCR-ABL1IS categories from the previous 2 assessments, and the proportion of previous BCR-ABL1IS observations at or below MR4. BCR-ABL1IS transcript levels for patients in the NIL and IM arms of ENESTnd were stratified into 5 clinically relevant categories: ≤ 0.0032% (MR4.5), > 0.0032% to ≤ 0.01% (MR4), > 0.01% to ≤ 0.1%, > 0.1% to ≤ 10%, and > 10%. The model was specified to be a second-order Markov chain (to accommodate previous BCR-ABL1IS transcript levels) with ordinal prediction values (for ordered BCR-ABL1IS categorical outcomes).
Results: Overall, 522 patients (NIL, n = 258; IM, n = 264) were included in the model, which contributed 5950 usable observations of BCR-ABL1IS transcript levels with corresponding values from the 2 prior assessments. Achievement of EMR (P = .0007), proportion of previous BCR-ABL1IS observations at or below MR4 (P < .0001), and BCR-ABL1IS categories from the previous 2 assessments (both P< .0001) were significant predictors of BCR-ABL1IS category at any time after 1 year of treatment. In our model, neither Sokal risk score nor type of therapy was a significant predictor of BCR-ABL1IS category due to their high correlations with other factors included in the model and which are measured on treatment. For example, more patients in the NIL arm than in the IM arm achieved EMR (91% vs 67%, respectively), which accounted for a lack of model statistical significance for treatment type. Model predictions had good agreement with the observed trial data (Figure).
Conclusion: Patients with CML who achieve EMR after initiating frontline TKI therapy have improved long-term treatment responses and survival outcomes. Our model also demonstrates that achievement of EMR is significantly associated with BCR-ABL1IS transcript levels after 1 year. These results add to the growing body of evidence that early response to TKI treatment should be carefully considered to ensure optimal long-term treatment success.
Saglio:Pfizer: Consultancy, Honoraria; ARIAD: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Novartis Pharmaceutical Corporation: Consultancy, Honoraria. Snedecor:Pharmerit International: Employment, Other: Institution received payment to conduct this study. Ji:Novartis Pharmaceuticals: Research Funding. Tai:Pharmerit International: Employment. Ray:Novartis Pharmaceutical Corporation/Rutgers University: Other: I am currently a fellow with Rutgers University, conducting my "field" experience at Novartis.. Mendelson:Novartis Pharmaceutical Corporation: Employment, Equity Ownership. Buchbinder:Novartis Pharmaceutical Corporation: Employment, Equity Ownership. Edrich:Novartis Pharma AG: Employment. Mahon:Novartis: Consultancy, Honoraria; Pfizer: Consultancy; ARIAD: Consultancy; Bristol-Myers Squibb: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal