Abstract
Background: Follicular lymphoma (FL) is the most frequent indolent lymphoma and is characterized by a high response to immunochemotherapy (ICT). However, patients refractory to first-line ICT have a worse prognosis. The objective of this study was to determine the prevalence of refractory FL, the factors that predict refractoriness as well as the salvage treatment and outcome.
Patients and methods: This is a retrospective analysis including stage II-IV FL patients treated with first-line ICT in 3 Spanish institutions. The cohort was divided into ICT-refractory patients (less than partial response after induction or maintenance/consolidation therapy, as well as relapse or progression within 6 months of the last dose of therapy) and ICT-sensitive. Baseline features, therapy received and outcome were analyzed.
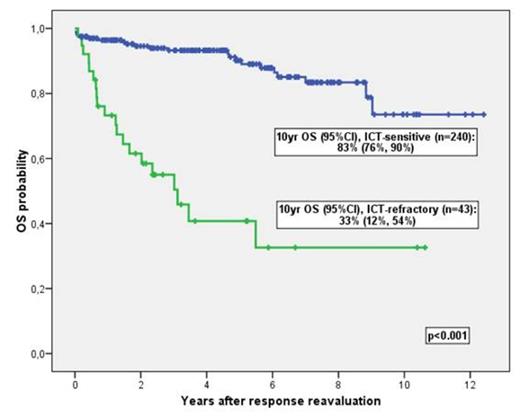
Results: 283 patients were included, the median age was 58 years-old (range 28 to 85) and 53% were female. 200/231 (87%) had a good performance status (ECOG < 2), 260/295 (88%) presented with stages III and IV and 163/284 (57%) had bone marrow involvement. High-risk FLIPI score was seen in 108/256 (42%), high serum LDH in 78/263 (28%) and high serum B2-microglobulin in 138/253 (54%). RCHOP was administered to 226 (80%), RCVP to 36 (13%) and rituximab in combination with fludarabine or bendamustine-based therapy to 21 (7%). Seventeen patients received consolidation with radioimmunotherapy and 140 received maintenance with rituximab (n=137) or interferon (n=3). Sixteen patients received complementary radiotherapy. Forty-three (16%) patients were ICT-refractory (37 within 6 months of the completion of induction and 6 during or within 6 months of the completion of maintenance/consolidation therapy). On univariate analysis, high-risk FLIPI (OR 5.4, [95% CI 2.3-12.6]), high-risk FLIPI2 (5.4, [2.4-12.4]), B symptoms (3.2, [1.6-6.6]), ECOG ≥ 2 (4.6, [2-10.9]), involvement of > 4 nodal regions (2.3, [1.02-5.3]), hepatomegaly (7.5, [2.6-21.5]), splenomegaly (2.8, [1.4-5.9]), high B2-microglobulin (4, [1.7-9.5]), high serum LDH (3.9, [1.8-8]) and treatment with RCVP (compared with RCHOP, 2.8, [1.2-6.2]) were correlated with refractoriness. On multivariate analysis, high-risk FLIPI score (4.9, [2.1-11.7]) and treatment with RCVP (3.4, [1.2-9.4]) were the only variables associated with refractoriness. After exclusion of FLIPI, ECOG ≥ 2 (3, [1.1-8.4]) and high serum LDH (4.7, [2-11]) were correlated with refractoriness, in addition to RCVP therapy (4.5, [1.5-13.2]). Ten-year OS probabilities in ICT-sensitive and ICT-refractory patients were 83% (95% CI 76%-90%) and 33% (12%-54%), respectively (p<0.001) (Figure 1). ICT-refractory patients were more likely to be also refractory to second-line therapies than ICT-sensitive patients (21/31 [68%] vs 10/58 [17%], p<0.001). In addition, histological transformation was suspected by clinical or biological features or confirmed by tissue biopsy in 11/43 ICT-refractory and 8/240 ICT-sensitive (p<0.0001). Death among ICT-refractory patients was more frequently due to lymphoma than in ICT-sensitive patients (19/23 [83%] vs 14/28 [50%], p=0.033).
Conclusions: In this series of FL treated with first-line ICT, the prevalence of refractoriness was low and occurred most frequently during or within 6 months of induction rather than maintenance/consolidation therapy. FLIPI score and RCVP treatment (compared to RCHOP) were predictive of refractoriness. The response rate of ICT-refractory FL patients to second-line therapy is low and the prognosis is poor.
Supported in part by RD12/0036/0029 del RTICC, Instituto Carlos III.
Overall survival in immunochemotherapy (ICT)-sensitive and ICT-refractory patients (p<001)
Overall survival in immunochemotherapy (ICT)-sensitive and ICT-refractory patients (p<001)
Sancho:CELLTRION, Inc.: Research Funding. Sureda:Seattle Genetics Inc.: Research Funding; Takeda: Consultancy, Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal