Abstract
Introduction: Approximately 20% of classical Hodgkin lymphoma (HL) patients are greater than 60 years old at diagnosis. The survival of this subgroup is inferior to that of younger patients, despite most being treated with curative intent. Possible reasons for this difference include: comorbidities, toxicity of treatment (especially bleomycin, Stamatoullas at al. BJH 2015), poorer baseline performance status, different disease biology, and more frequent chemotherapy dose reductions. Recent advances and refinements in treatment have not improved the outcomes of elderly patients with HL significantly (Johnson and McKenzie. Blood 2014). Selection of a regimen for HL should take comorbidities into account. There is not a clear standard of care treatment regimen for elderly patients with HL.
Methods: Patients were treated by physicians of the Nebraska Lymphoma Study Group between 6/1983 and 6/2014. There were 119 patients with biopsy-proven HL who were 60 years of age or older at the time of diagnosis. The Kaplan-Meier method was used to estimate overall survival distributions and the log-rank test was used to compare survival distributions between groups. Comparisons of survival distributions were made using the log-rank test. Chi-square tests and t-tests were used to compare outcomes by treatments received. P-values less than 0.05 were considered to be statistically significant.
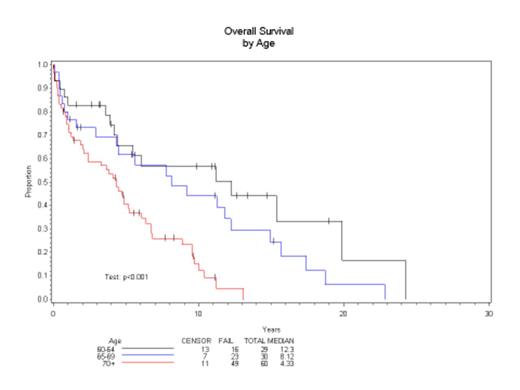
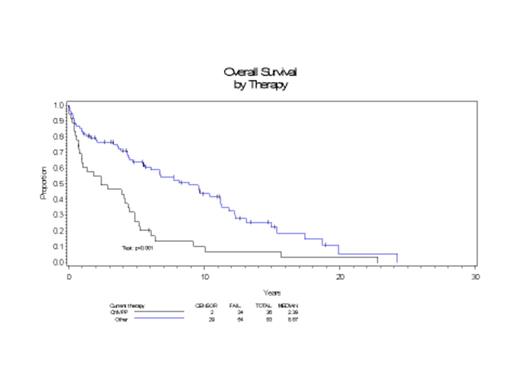
Results: The mean age was 71 years (range 60.1 to 89.2). Mixed cellularity was the most common histological subtype (28.57%). Therapies given included: non-anthracycline based regimen ChlVPP in 36 patients (30.25%) and radiotherapy alone in 13 patients (10.92%); and anthracycline containing regimens ChlVPP-ABV in 35 patients (29.41%), Stanford V in 9 patients (7.56%) and ABVD in 26 (21.85%). Patients older than 70 did significantly worse OS p<0.001 (Figure 1). OS was not different with regards to stage at diagnosis I/II vs III/IV (p=0.3). Patients receiving an anthracycline containing regimen had a better OS than those receiving ChlVPP alone p<0.001 (Figure 2). In both, early stage (I-II) and late stage (III-IV) HL the best outcomes were seen either ABVD or ChlVPP-ABV. OS was inferior in patients who did not receive bleomycin or in those for whom it was stopped, as opposed to patients receiving full bleomycin planed doses p=0.029. Bleomycin was omitted in 6/70 patients, generally as a result of preexisting pulmonary comorbidities. Bleomycin was stopped/held during treatment in 18 patients (28.1%) because of concerns of toxicity. There were no deaths with a diagnosis of bleomycin lung injury in our series.
Conclusions: HL patients performed worse with increasing age and patients above 70 years of age had a median survival of 4.6 years. Anthracyclines seem to be essential for optimal outcome, confirming a previous publication by our group (Weekes at al. JCO 2002). Either ABVD or ChlVPP-ABV appear to be equally effective in patients who can tolerate an anthracycline. Our results appear to compare favorably to other regimens tested in elderly HL patients: VEPEM-B tested in the UK (Proctor et al. Blood 2012) and the PVAG tested by the German group (Boll et al. Blood 2011). Although bleomycin is difficult to give to this population because of increased toxicity, patients who did not receive bleomycin or had it stopped during treatment had a poorer survival. Our results confirms the results of a recent publication from the German Group in which bleomycin omission in early-stage HL patients performed worse (Behringer at al. Lancet 2015). Certainly bleomycin is associated with pulmonary toxicity in this age group, although our incidence was not as high as reported in the North American Intergroup Trial (43%) with bleomycin administration for HL patients (Evens, Br J Haematol 2013). Though limited by the possible occurrence of selection bias conferred by the retrospective design, anthracycline-based regimens appear to be associated with better outcomes in elderly patients with HL.
Lunning:TG Therapeutics: Consultancy; Genentech: Consultancy; Gilead: Consultancy; Juno: Consultancy; BMS: Consultancy; Spectrum: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal